A new study shows that defects of the skull, face, or jaw bone might benefit from reconstructive surgery that uses stem cells taken from adipose tissue seeded on resorbable scaffolds.
These defects can be due to congenital malformations, such as cleft lip and palate, or traumatic injuries or surgery to remove a tumor. The use of a patient's own bone is still considered the gold standard for reconstructing these defects, but this requires yet another surgery to harvest the bone for the reconstructive procedure. The study, published in Stem Cells Translational Medicine (February 20, 2014), tracked the cases of 13 patients undergoing regenerative medicine procedures.
The study represents the first application compliant with good manufacturing practices (GMP) for autologous adipose-derived stem cells in the treatment of defects at various sites of the craniomaxillofacial skeleton, noted study investigator George Sándor, MD, DDS, PhD, of the University of Tampere (UT) in Finland. He and Susanna Miettinen, PhD, were lead investigators on the study conducted by scientists and clinicians who, in addition to UT, came from the University of Oulu in Finland and Central Hospital in Jyväskylä, Finland.
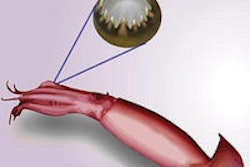
Isolated reports of hard-tissue reconstruction in the skull, face, or jaw exist, but multipatient case series are lacking. This study aimed to review the experience of 13 people with hard-tissue defects at four anatomically different sites: the frontal sinus (three cases), cranial bone (five cases), the jaw (three cases), and the nasal septum (two cases).
Stem cells were harvested from adipose tissue in each patient's abdomen, treated in the lab and then seeded onto resorbable scaffold materials for implantation back into the patient. The scaffolds were constructed with either bioactive glass or β-TCP, a bone graft substitute. In some cases a protein called rhBMP-2, which plays an important role in the development of bone and cartilage, was added, too.
The results were promising. All three of the frontal sinus cases and three of the five cranial defect cases were successfully treated. One of the two septal perforations failed after a year due to an infection resulting from the patient's own actions, but the other healed successfully.
The three patients with reconstructed jaw defects also had good results; in fact, two of them chose to have dental implants placed directly into the stem cell-seeded grafts after healing, allowing these patients to once again enjoy a normal diet.
While the resorption of some of the constructs in the cranial defects was more than expected, the majority of these challenging defects (10 of 13) were successfully treated with integration of the stem cell-seeded constructs to the surrounding skeleton at the defect sites, the researchers noted. They added that the next steps should involve more animal studies and tracking of long-term results in humans.