Dentists are expected to perform at a high level at all times. Our work begins when we examine a patient and formulate a diagnosis for a problem they are experiencing or treatment plan a comprehensive dental case.
Determining what is normal versus what is diseased becomes routine with the use of cone-beam CT (CBCT) imaging. I use a Galileos CBCT system (Sirona Dental) to discover abnormal tissue by revealing and identifying unusual findings or signs in the maxillofacial anatomy of my patients.
It is quite common to scan a patient for diagnostic purposes in one area and discover pathology or atypical anatomy in a different area. An incidentaloma -- a term coined in a 2010 article in the Journal of Implant & Advanced Clinical Dentistry (April 2010, Vol. 2:3, pp. 87-92) is the "discovery of any unsuspected pathology, anomaly, dental structure (such as retained root tip, impacted tooth, or supernumerary), or deviation from the normal anatomy on a CT scan."
Extensive decay, periodontal disease (bone loss), endodontic pathology, missed canals, sinus pathology, internal resorption, and missing teeth are common findings during a complete dental examination. Enhanced imaging CBCT scans reveal these problems at such a high rate that some practices routinely scan all their patients, because many of these problems go unseen in limited 2D radiographs. I am not a proponent of that practice.
I will present a number of scans that illustrate extensive asymptomatic pathology and bony destruction that goes undetected, unrecognized, or neglected by dentists and patient alike. Assessing 3D scans with the patient improves communication and increases case acceptance. Patients with low dental IQ can be informed and persuaded that deleterious pathologies need to be removed and tissue restored.
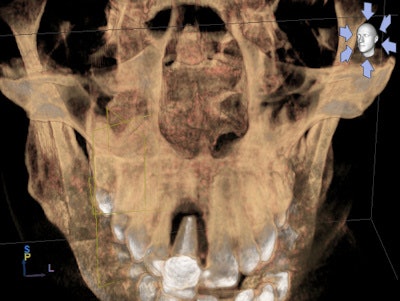
Case No. 1
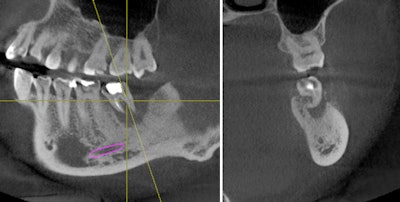
 Hopeless tooth #19. All images courtesy of Dr. Anthony Ramirez.
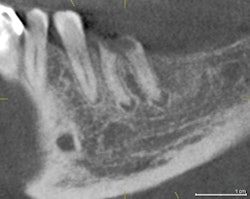
Hopeless tooth #19. All images courtesy of Dr. Anthony Ramirez.A 63-year-old male patient was informed numerous times over the past 10 years that periodontal disease was destroying the bony support for both maxillary first molars. All previous treatment plans were declined.
During an emergency visit, he presented with a crown that became dislodged from tooth #19. Teeth were asymptomatic, but the loss of this crown convinced him to accept an enhanced CBCT scan to diagnose the area of #19.
On review of his 3D images, it became apparent that neglecting to intervene earlier had allowed periodontal hard-tissue breakdown to progress to an unmanageable state for tooth #3 and possibly for tooth #14. Tooth #19 was deemed hopeless and could be extracted, bone grafted, implanted, and restored, as the bone volume could be regenerated to receive an implant.
 Expanding perio-endo pathology.
Expanding perio-endo pathology.The incidental findings in this scan were multiple: the total resorption of palatal bone in the area of tooth #14 with periapical pathology, and the complete destruction of alveolar support for tooth #3, which was close to undermining the apices of the adjacent premolar #4. The treatment plan was formulated based the images shown.
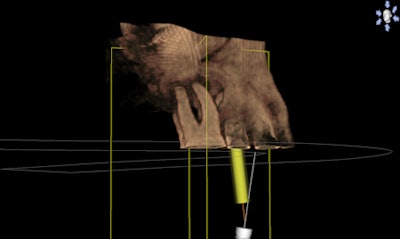
 Bone pathology on #3.
Bone pathology on #3.Extensive bone grafting would be necessary to restore the bone in the areas of #14 and #19 if there were to be any thought of replacing these teeth. I extracted both teeth and bone grafted.
I used a mineralized freeze-dried bone, Puros, to fill in all of the bone defects and act as a scaffold for the regeneration of alveolar bone. The particles are a cortical-cancellous mixture and are covered by a resorbable barrier membrane that contains the graft and maintains space. The success of this procedure depends on the removal of all diseased tissue, degranulation, and decortication of the medullary bone, which creates the blood supply necessary for bone growth factors. I usually wait a minimum of three months before re-evaluating the bone graft for preimplant planning.
 Extract, bone graft, and implant on #14 and #19.
Extract, bone graft, and implant on #14 and #19.Case No. 2
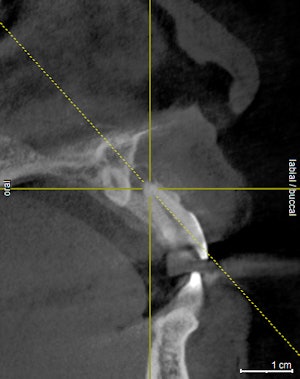
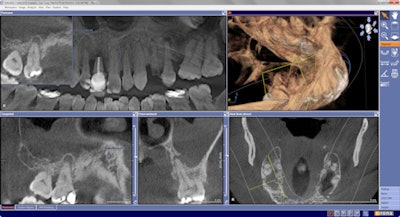
A 29-year-old woman presented for examination and consultation to diagnose a mildly symptomatic lower left second molar. Her previous dentist recommended she visit an endodontist for retreatment of this tooth.
Oral exam revealed a lower left second molar tooth with class III mobility and severe occlusal wear. Periapical pathology was present because of a poorly treated root canal. A CBCT scan gave us a clear understanding that tooth #18 was hopeless and was literally floating in pathology.
 Left: Perio-endo lesion on #18. Right: Cross-sectional view of #18.
Left: Perio-endo lesion on #18. Right: Cross-sectional view of #18.Incidental findings were present: a mesiodens in the area of #9 with an associated asymptomatic periapical lesion.
 Mesiodens and periapical pathology, #9.
Mesiodens and periapical pathology, #9.This patient was a medical professional and was thankful for the level of expertise that we provided her, and she moved forward with the extraction, bone graft, implant, and restoration of tooth #18 that was necessary to return her to a full complement of teeth.
 Regenerated bone preimplant, #18.
Regenerated bone preimplant, #18.This is another example of the way CBCT imaging enlightens our patients and gives them a basis for treatment that they otherwise would not have.
 Implant restored.
Implant restored.Case No. 3
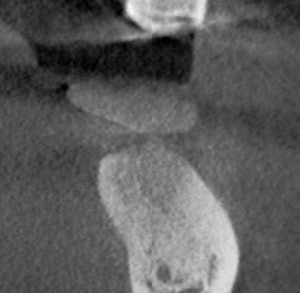
A 45-year-old man presented for a consultation regarding his loose front tooth. How this tooth did not exfoliate was beyond belief as it was being held in by only granulation tissue.
Multiple dentists had examined him during the preceding six months, but he wasn't comfortable with their methods, technology, or facilities. A Google search led him to our office, specifically because of our Galileos CBCT scanner.
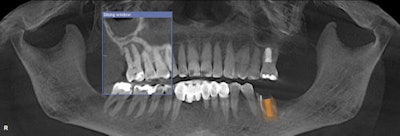
Preliminary diagnostic methods were completed, and we discussed how a scan could improve my diagnosis and treatment plan. I wanted to see the whole picture and use the 3D images to fully inform him as to the options available for replacing tooth #8.
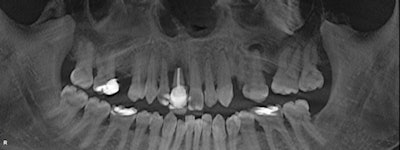 Above: Initial panoramic image. Below: Pathology on #8 and #13.
Above: Initial panoramic image. Below: Pathology on #8 and #13.The CBCT images were impressive and became the foundation for my complete dental examination. Incidentalomas were numerous: multiple periapical pathologies and moderate to severe periodontal disease. Although he presented for his maxillary incisor, I was able to capture his attention and devise a pragmatic plan to improve the overall prognosis for his entire dentition.
 Above: Exfoliating max central incisor. Below: Pathology on #12 and #13.
Above: Exfoliating max central incisor. Below: Pathology on #12 and #13.A challenging road lay ahead as multiple disciplines of dentistry would be necessary to return a poorly maintained dentition to a healthy fully functioning one. Note that multiple asymptomatic periapical lesions existed with #3, #12, #13; multiple teeth were missing; and there was generalized severe periodontal breakdown.
 Above: Incidentalomas on #3 and #13. Below: Sinus pathology in right sinus and periodontal disease.
Above: Incidentalomas on #3 and #13. Below: Sinus pathology in right sinus and periodontal disease.The value of the CBCT imaging in this case went well beyond the diagnostic benefit by enhancing communication and aiding case acceptance for a patient who had finally made up his mind to seek help and improve his dental health.
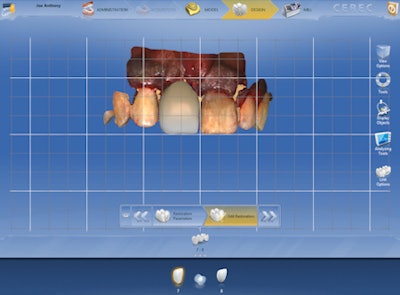 Proposal to replace #8.
Proposal to replace #8.The next article will illustrate how Cerec CAD/CAM can provide the basis for computer-assisted guided implantology.
Anthony Ramirez practices in Brooklyn, NY. He can be reached at [email protected] or via his website.
The comments and observations expressed herein do not necessarily reflect the opinions of DrBicuspid.com, nor should they be construed as an endorsement or admonishment of any particular idea, vendor, or organization.