Zirconia received satisfactory marks in a new review of systematic reviews of the restorative material. While zirconia-ceramic restorations came with technical, biological, and aesthetic complications, many of these complications did not affect restoration functionality and could be fixed during routine care.
Zirconia is one of the most popular tooth-colored restoration materials, but the technology and aesthetics have improved over time. The new qualitative review summarized the evidence on the restorative material over the past 16 years, with the authors concluding the reviews showed "satisfactory results."
"The predominant technical problem of veneering fractures could be overcome with adapted design or fabrication and the application of monolithic restorations," wrote the group, led by Harald Laumbacher from the department of prosthetic dentistry at University Hospital Regensburg in Germany (Journal of Dentistry, June 11, 2021).
The authors searched multiple scientific databases and included 38 systematic reviews in their own review. Their qualitative analysis benefited from the combined findings of 128 individual primary studies with about 10,000 zirconia restorations. The reviews ranged in date from 2006 to 2021 and reported on survival, success/failure, and complication rates.
Survival rates were high for various types of zirconia restorations. In follow-up time frames ranging from six months to 11 years, zirconia single crowns had survival rates of 75% to 100%, while multiunit fixed dental prostheses (FDPs) had rates of 67% to 100%. Studies that compared all-ceramic single crowns with metal-ceramic crowns found that the five-year survival rate for zirconia crowns was 91%, compared with 96% for metal-ceramic crowns.
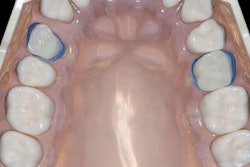
Chipping and framework fracture were the most frequently reported technical compilations for zirconia restorations. Among these complications, fracture of the veneering material was the prevalent technical failure. Other frequently reported complications included loss of retention and marginal discrepancies.
"The incidence of ceramic fractures (chipping and fractures) and loss of retention was significantly higher for densely sintered zirconia FDPs," the authors wrote.
Fortunately, chipping and veneer fractures tended to be minor and correctable with polishing or slight repair. In fact, many patients only learn of chipping during routine appointments, the authors noted.
Zirconia restorations also failed for biological reasons, including secondary caries, the need for endodontic treatment, abutment tooth fracture, periodontal disease, and persisting pain. Multiple studies noted a loss of vitality for densely sintered zirconia FDPs, the authors wrote.
To zirconia's merit, few studies reported aesthetic complications with the material. In fact, color mismatch was the only aesthetic complication mentioned in the included reviews.
The majority of the reviews were of high quality and had low risk of bias. However, the authors cautioned that the most extensive reviews lacked detailed information on the dental materials used. Many of the primary studies also excluded patients with bruxism, which is common in the general patient population and can affect crown survival rates.
"Beside this, other parafunctional habits, temporomandibular disorders, or the impact of zirconia based prosthodontic restorations on the masticatory system on the functional or anatomical level in general were not addressed," they noted.
With these limitations in mind, the authors called on future researchers to conduct studies in people who have conditions regularly found in the general population. They also noted researchers should investigate the long-term effects of zirconia on the larger stomatognathic system.
"Further studies are required in this regard," the group concluded. "For this purpose, uniform evaluation criteria should be established."