A 62-year-old woman developed a life-threatening presence of air within her skull when a dental clinic used an air-polishing device to perform submucosal debridement to treat her peri-implantitis lesion, according to a case report published May 3 in Clinical and Experimental Dental Research.
Two seconds after the device was turned on, the patient complained of extreme discomfort in her face and head. Computed tomography (CT) scans revealed air in the woman's intracranial space, a phenomenon referred to as pneumocephalus.
Because the air was likely contaminated with oral bacteria, the patient was in danger of developing meningitis, the authors wrote. She was immediately admitted to the hospital and recovered following antibiotic treatment.
"The present case of direct development of pneumocephalus from a dental procedure is the first in the literature, and thus it should be regarded as an extremely rare complication," wrote the authors, led by Dr. Corinna Bruckmann of the division of conservative dentistry and periodontology, University Clinic of Dentistry, Medical University of Vienna, in Austria.
Very rare complication
In 2019, a 62-year-old woman with no remarkable health problems enrolled in a routine program for treatment of peri-implantitis at the Medical University of Vienna. Five years earlier, she had a sinus floor elevation procedure around tooth #26 and #27. Postoperative healing was uneventful, and two implants were placed.
At the time of presentation in 2019, the woman had probing pocket depths of 6-7 mm, bleeding on probing, and pus discharge in the area of the implants. In the following months, she received two rounds of nonsurgical peri-implantitis therapy with handsonic and ultrasonic instruments in addition to adjunct systemic and local antibiotics.
The woman's care was then interrupted by the COVID-19-related pandemic lockdowns. When she returned to the program in March 2021, her pocket depth was once again 7 mm at implant #27. The clinic chose to remove her supragingival and subgingival biofilm using an air-polishing device with a supragingival handpiece and an erythritol-based powder.
Following manufacturer recommendations, the device was positioned at a 60° angle at a distance of 3-5 mm toward the gingival sulcus. It was set at 100% water flow and 40% power and had a sterile disposable nozzle.
The nozzle was inserted mesially at a depth of 7 mm with implant #27, and the device was activated. After two seconds, the patient reported extreme discomfort in the left side of her face and head, and the treatment was stopped.
The patient was placed in an upright position. She was awake and oriented, reported minimal shortness of breath, pain behind the left eye, and difficulty swallowing. Her blood pressure, heart rate, and light pupil reaction were normal. Extraoral and intraoral exams revealed nothing unusual.
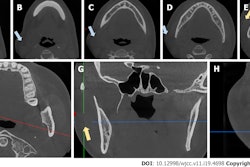
Due to the strange sensations reported by the patient and unclear clinical signs, the patient underwent a CT scan, which showed the development of a subcutaneous emphysema. The air spread from the facial aspect in caudal and cranial directions. Air was also detected in the left carotid canal and intracranially, according to the report.
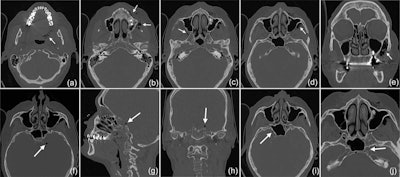
A CT scan revealed that the subcutaneous emphysema extended to the woman's left side pharyngeal (a) and facial (b) into the right (c) and left (d) pterygopalatine fossa, with a maximum extension of up to 3 cm on the left side (e). The intracranial air bubbles reached a diameter of up to 5 mm (axial [f], sagittal [g], and coronal [h] view). The bubbles were detected on both sides of the sella turcica in the region of the cavernous sinus (i) and on the left side in the carotid canal (j). Images courtesy of Bruckmann et al. Licensed by CC BY 4.0.
Due to the risk of meningitis, the woman was immediately admitted to the hospital. She was closely monitored and given intravenous antibiotics three times per day. A CT scan revealed that the pneumocephalus had resolved and the soft-tissue emphysema had regressed. She was discharged three days after admission with a five-day prescription for oral antibiotics. Her recovery was unremarkable, the authors noted.
A few months after her hospital stay, the woman's pocket depth had worsened on implant #27, and she chose to have it removed. The surgery and postoperative healing were uneventful.
Identifying a possible cause
Since 1960, there have been reports of approximately 150 cases involving patients developing dental procedure-related subcutaneous emphysema. It has been described in diverse locations, including the mediastinum and orbital region, and many have occurred after the use of high-speed handpieces and air syringes.
This is believed to be the first case of pneumocephalus developing during submucosal debridement of a peri-implantitis lesion with an air-polishing device. The authors suspect bone defects may have played a role in this specific case.
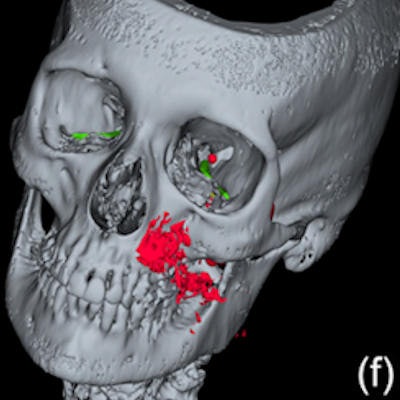
The woman's CT scans showed a deep peri-implant bone defect at the mesial aspect of implant #27 that extended almost into the sinus space, as well as a bone defect at the sinus wall, which was likely a remnant from the woman's prior sinus floor elevation procedure.
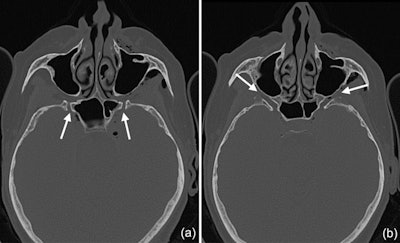
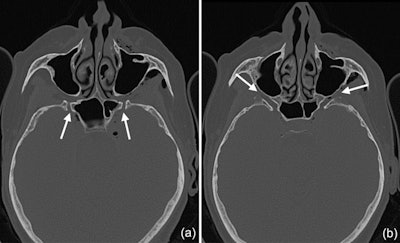
CT scans show that the pterygoid canal (a) and the forum rotundum (b) may be possible entry pathways for the air to enter the intracranial space. This is especially possible within the canal leading to the foramen rotundum, where several smaller air bubbles were captured.
"Hence, as the nozzle was inserted at the mesial aspect of the implant, the compressed air could have extended along the peri-implant defect into the augmentation material and then exited via this residual bone defect in the lateral sinual wall and into the surrounding soft tissue of the facial aspect of the posterior left maxilla," the authors wrote.
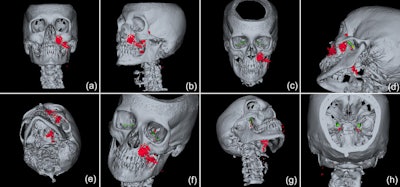
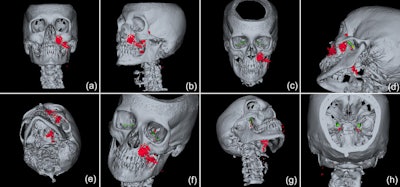
3D reconstructions of the emphysema (red) and the display of the potential pathways to the intracranial space, including along the inferior orbital fissure and via the foramen rotundum (green) and/or via the pterygoid canal (yellow).
Since more patients are getting implants, peri-implant complications are becoming more frequent, as is the use of air-polishing devices to manage these conditions. Therefore, clinicians should expect emphysemas to occur more often, the authors wrote.
More studies are needed to provide evidence-based recommendations for the use of air-polishing handpieces in the treatment of peri-implantitis. Also, more extensive imaging should be considered when a subcutaneous emphysema is identified so that the risk of complications can be assessed, the authors wrote.
"It is suggested that in case of an extensive subcutaneous emphysema, a more extended radiographic examination including the cranial and mediastinal space should be considered as standard examination, to assess the risk of potential life-threatening complications," Bruckmann and colleagues concluded.