Periodontal pocket depth is traditionally measured with a periodontal probe, but many factors can distort this measurement. What if there were a way to image these pockets with a cone-beam CT (CBCT) system so you knew the depth precisely?
Researchers from Georgia wanted to discover if a CBCT system (i-CAT Next Generation, i-CAT) could produce an accurate 3D analysis of periodontal pockets. They found that this method was both accurate and plausible, but they also cautioned that much more research and testing were necessary.
"This approach could transform the diagnosis and treatment planning of periodontal disease, with particular initial utility in complex cases," wrote the authors, led by Mahmoud Elashiry, an oral biology graduate student at the Dental College of Georgia at Augusta University (Dental Materials, February 4, 2018).
Pocket analysis
Measuring a patient's periodontal pockets is typically done with a periodontal probe. However, measurements may vary among practitioners because of the probe's shape and angle, the degree of inflammation, and other reasons. The probe also does not provide 3D information about the pocket.
“This approach could transform the diagnosis and treatment planning of periodontal disease, with particular initial utility in complex cases.”
Researchers wanted to determine if a conventional CBCT system could be used to accurately analyze these pockets. They tested the idea using a pig jaw model with alveolar bone loss and surgically induced periodontal pockets, as well as a human skull model with artificial gingiva applied to teeth with alveolar bone loss and calibrated pockets. They also measured the pockets using a probe.
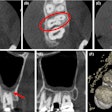
The researchers injected a radiopaque microparticle filler, composed of calcium tungstate in a glycerol-water solution, into the pockets. Then they took images of 12 pocket sites (six teeth each with two pockets) in the pig jaw and 62 pocket sites (31 teeth each with two pockets) in the human skull model.
Rather than provide actual pocket measurements, which would not be relevant as they were artificially created, the researchers compared the pocket depth and volume measurements made manually with those made with the CBCT system to see if there was an agreement between measurements.
They reported significant intermethod agreement (95% confidence interval [CI], 0.938-0.991) and intramethod agreement (95% CI, 0.94-0.99) when comparing the periodontal probe measurements with the digital CBCT measurements.
Initially, the researchers were concerned about the potential effects of artifacts (beam hardening, scattering, and metallic artifacts) on CBCT imaging.
"However, this study suggests that there was little impact of such artifacts that could be created from radiopaque fillers delivered into [the pockets] and amalgam restorations on CBCT pocket imaging," the study authors wrote.
Improving diagnosis
The authors cautioned that this was only the first step in this research. Another limitation of the study was that both the pig jaw and human skull models lacked crevicular fluid and saliva.
"Validation of the practicality of this new technology is needed in living animal models and in clinical trials in periodontitis patients," they noted.
Nevertheless, these results validated the idea that this was a plausible means of measuring the depths, volumes, and 3D shapes of these pockets, the authors concluded. Efforts to confirm the clinical practicality of these fillers are currently in progress, they added.
"The results of the current study proved the concept of accurately visualizing the periodontal pocket morphology with its soft-tissue component three dimensionally," the authors wrote. "That, in turn, may help dentists in improving their periodontal diagnosis and prevent underestimation of the pocket extension that is common to happen with the current periodontal probing method."