Imaging aided in managing a man’s atypical root canal anatomy in which the distobuccal canal of his maxillary second molar was close to the palatal root canal with partially fused roots. The case report was published on May 5 in Clinical Case Reports.
From the clinical and imaging findings, clinicians diagnosed the man with pulpal necrosis with symptomatic apical periodontitis and then executed appropriate endodontic treatment, the authors wrote.
“For successful endodontic treatment, clinicians should be aware of the variations in the number of roots and root canals and the peculiar or eccentric location of root canals as described in this case report,” wrote the authors, led by Dr. Anand Marya of the department of orthodontics and dentofacial orthopedics at the University of Puthisastra in Cambodia.
Varying root canal systems
Root canal anatomy is highly complex and variable, with most differences being in the form of extra canals. The literature has reported variations in maxillary second molars in the number of roots and root canals. To ensure the best possible endodontic treatment outcomes, clinicians should know about canal differences, according to the report.
A 34-year-old man with tooth pain
A 34-year-old man visited a clinician after experiencing reported intermittent localized throbbing pain in upper left back tooth for 10 days. The pain occurred during the night and was aggravated during chewing. An intraoral exam revealed deep occlusal caries in the maxillary left second molar, and the tooth had an old amalgam restoration on the occlusal surface.
Thermal and electric pulp testing elicited a negative response, and an x-ray showed occlusal radiolucency that involved the pulp space with no periapical radiolucency. Based on the exam and imaging, a diagnosis of pulpal necrosis with symptomatic apical periodontitis was made, and the man underwent endodontic treatment, the authors wrote.
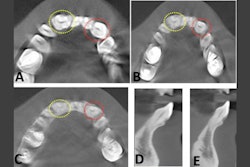
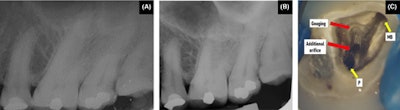 (A, B) The preoperative intraoral x-ray of the man’s maxillary left second molar. (C) Pulp chamber floor of the tooth showing the presence of an additional orifice in close approximation relation to the palatal (P) orifice and subsequent gouging in the distobuccal region adjacent to the mesiobuccal (MB) orifice.Images courtesy of Marya et al. Licensed by CC BY 4.0.
(A, B) The preoperative intraoral x-ray of the man’s maxillary left second molar. (C) Pulp chamber floor of the tooth showing the presence of an additional orifice in close approximation relation to the palatal (P) orifice and subsequent gouging in the distobuccal region adjacent to the mesiobuccal (MB) orifice.Images courtesy of Marya et al. Licensed by CC BY 4.0.
The patient’s pulp chamber floor was examined with an endodontic explorer, which revealed three distinct root canal orifices: the mesiobuccal, palatal, and another orifice in close approximation to the palatal canal. It appeared that there was an extra palatal canal. While attempting to search for the distobuccal canal in its usual position, the floor in that area was gouged, they wrote.
Since the distobuccal canal was not located in its usual location and a canal was seen in an unusual place between the buccal and palatal canals, a limited field of view cone-beam computed tomography (CBCT) scan was taken. The 3D images of the maxillary second molar revealed that the buccal and palatal roots in the coronal and middle third region of the root were fused. However, they were separated apically.
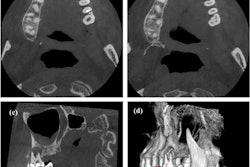
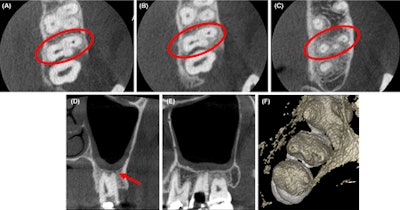 (A-C) Axial CBCT images in the cervical, middle, and apical region of the man’s molar. (D) The coronal section showed the apical split of roots and early periapical radiolucency in the palatal root (red arrow). (E) The sagittal section shows the gouging of the floor.
(A-C) Axial CBCT images in the cervical, middle, and apical region of the man’s molar. (D) The coronal section showed the apical split of roots and early periapical radiolucency in the palatal root (red arrow). (E) The sagittal section shows the gouging of the floor.
Also, the CBCT images confirmed that the distobuccal canal was adjacent to the palatal orifice. The scan further revealed that the coronal section of the tooth had early periapical radiolucency in the palatal root, which was not visible on the early images, the authors wrote.
With a clear visualization of the tooth’s canals, clinicians executed the endodontic procedure. About two weeks after the procedure, the patient was asymptomatic, they wrote.
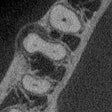
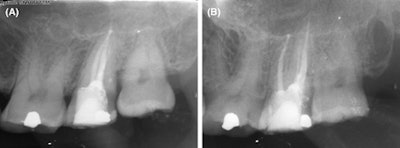 (A) Patient x-ray immediately after surgery. (B) Patient x-ray one year after surgery.
(A) Patient x-ray immediately after surgery. (B) Patient x-ray one year after surgery.
Since spatial relationships between the roots and adjacent anatomical structures, as well as their shapes and positions are often difficult to assess using x-rays, a CBCT scan can provide a better understanding of internal root canal anatomy, the authors wrote.
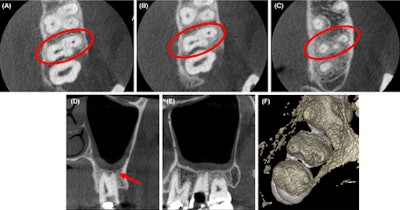
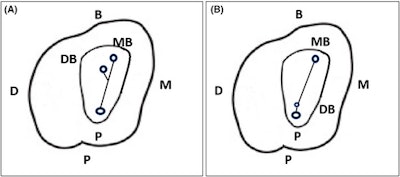 (A) An illustration of the typical location of the distobuccal (DB) root canal orifice in relation to the mesiobuccal (MB) and palatal (P) root canal orifices. (B) An illustration of the unusual location of the DB root canal in close approximation of the P root canal. (B, buccal; D, distal; M, mesial.)
(A) An illustration of the typical location of the distobuccal (DB) root canal orifice in relation to the mesiobuccal (MB) and palatal (P) root canal orifices. (B) An illustration of the unusual location of the DB root canal in close approximation of the P root canal. (B, buccal; D, distal; M, mesial.)
"Clinicians should be aware of the variations in the number of roots and root canals and the peculiar or eccentric location of root canals,” Marya et al wrote.