A patient comes into your office complaining of dry mouth, some swelling under the tongue, and associated pain at mealtimes. After a brief examination, you suspect a blockage of the submandibular gland and decide to refer the patient out to a radiologist to determine the cause of the obstruction.
In Europe, most likely the radiologist will call for an ultrasound. In the U.S., a computed tomography (CT) scan is more typical. Other options include conventional radiographs, sialography, and magnetic resonance imaging (MRI). All of these methods have their pros and cons:
Ultrasonography: Cost-effective and least invasive, but sensitivity in detecting salivary stones is only 75% and failure has been reported in cases of small, semicalcified stones (Fogorvosi szemle, April 2007, Vol. 100:2, pp. 53-58).
Conventional radiography: Cost-effective and readily available, but sensitivity rates are only about 60% (Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology, April 1992, Vol. 73:4, pp. 434-440).
Sialography: Can be used for direct radiographic evaluation of the ducts following injection of radiopaque dye, but invasive and contraindicated in patients with active infection (Radiology, September 2000, Vol. 216:3, pp. 665-671).
CT scan: Able to detect stones as small as 2 mm in diameter (typically 3-4 mm), but with higher radiation doses than other imaging modalities.
MRI: Good sensitivity (especially when combined with control radiographs), but higher cost.
"The difficulty with ultrasound is it is more operator-dependent," said M. Boyd Gillespie, M.D., M.Sc., an associate professor of otolaryngology and head and neck surgery at the Medical University of South Carolina. "A thin-cut CT scan captures the entire field of the gland, but with ultrasound the operator has to personally scan the gland and identify the stone."
And in addition to the insensitivity of radiographs -- "you may miss up to 30% of stones," Dr. Gillespie said -- there is the risk of radiation exposure.
"You have to worry about radiation exposure with CT also, but it's worth it if you can get a diagnosis," Dr. Gillespie said. "With plain film, one out of three or more patients would have to get a follow-up CT anyway."
Another alternative
Now a new study suggests that, when it comes to imaging salivary stones, cone-beam CT (CBCT) is equal in sensitivity and specificity to CT and offers lower radiation dosages (Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology, July 2010, Vol. 110:1, pp. 94-100). In fact, the study authors believe cone-beam CT represents "the preferable imaging modality for salivary calculus diagnosis" due to its "superior diagnostic performance and favorable information-to-radiation-dose ratio."
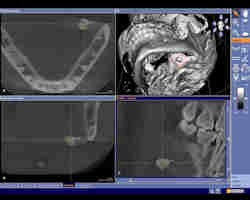
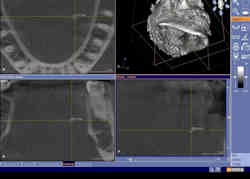
Timo Dreiseidler, M.D., D.M.D., and colleagues from the University of Cologne set out to evaluate the image quality and artifact influence of 29 cone-beam CT images containing salivary calculi. All images were acquired using a Galileos system from Sirona Dental Systems. As a control, an additional 29 cone-beam CT images from patients with no visible calculus were also evaluated.
 |
| Click here to enlarge this image. |
|
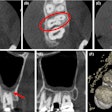
Cone-beam CT dataset showing a slightly overaverage size salivary calculus of 7-8 mm in the left submandibular gland area in the axial (upper left), coronal (lower left), and sagittal (lower right) view. Maximal diameters were measures using the visualization software tools. In the 3D reconstruction (upper right), the reformatted 3D salivary calculus is visualized and marked with a red circle. All images courtesy of Timo Dreiseidler, M.D., D.M.D., University of Cologne. |
 |
| Click here to enlarge this image. |
|
Cone-beam CT dataset showing a 2-mm salivary calculus in the left submandibular gland area in the axial (upper left), coronal (lower left), and sagittal (lower right) view. Clinical and conventional 2D diagnosis failed here due to the small size of the calculus. |
The researchers found that salivary calculi were sufficiently visualized in all patients and that the cone-beam CT measurements were highly reproducible, with mean differences of less than 350 microns. The mean difference between ultrasonography and cone-beam CT measurements was about 0.5 mm, whereas the mean difference between histomorphometry and cone-beam CT measurements was about 1 mm.
"Even the smallest calculi of 2 mm were visualized with the CBCT datasets," Dr. Dreiseidler stated in an e-mail to DrBicuspid.com. "In fact, standard resolution of CBCT datasets in general is higher than those of medical CT datasets. So, while the smallest voxel of cone-beam CT devices range from 100 to 300 microns, most commonly used medical CT protocols routinely have layer thicknesses of approximately 2 mm." That is why even the smallest salivary calculi can sometimes be depicted even better with cone-beam CT than with medical CT, he noted.
Dr. Dreiseidler was also impressed by the mean sensitivity and specificity of the cone-beam CT images: both 98.85%.
"We wondered if cone-beam CT could challenge already established standards and cope with the sensitivity of medical CT investigations," he said. "We found that cone-beam CT's sensitivity and specificity are close to 100%, which is uniquely superior to the standard diagnosis so far."
Lower radiation dosage
In addition, Dr. Dreiseidler noted, if cone-beam CT devices with low radiation dosages are applied, the information-to-radiation-dose ratio justifies routine use of this modality in salivary calculus diagnosis.
"A 0.6-mm voxel, midfacial medical CT investigation results in a 35-fold higher radiation dose to patients compared with digital panoramic tomography," the researchers wrote. "In contrast, the cone-beam CT device used in our study results in only a threefold higher dose [compared with] digital panoramic tomography."
In the past, if the estimated clinical diagnosis did not correlate with the ultrasound or conventional radiography findings, patients often were referred to medical CT or sialendoscopy -- both of which have disadvantages in terms of availability, invasiveness, emitted radiation dose, and investigation costs, Dr. Dreiseidler noted.
While sialoliths alone may not be common enough to warrant purchasing a cone-beam CT system -- only 1% of patients who present to dentists suffer from problems related to sialoliths -- "the holistic 3D cone-beam CT diagnosis opportunities, with its huge variety of proper indications for the dental practice, can increasingly lead to the general displacement of conventional radiographic technologies," he concluded.
Dr. Gillespie acknowledged that the study does make a case for the use of cone-beam CT in this application.
"They are not claiming that cone-beam CT is better than thin-cut CT scans," he said. "I think they are stating that its main advantages are that it is highly accurate, uses less radiation that standard CT scans, and is readily available in the office of some dentists and oral surgeons. Based on this information, it does appear to be a reasonable method for diagnosing sialoliths."
Copyright © 2010 DrBicuspid.com