Assessing root overlap with the maxillary sinus may predict the likelihood of the complication oroantral communication (OAC) after maxillary tooth extraction. This study was recently published in Clinical Oral Investigations.
Furthermore, the extent of root projection over the maxillary sinus may be positively correlated with the occurrence of OAC, the authors wrote.
“Fraction of the root overlapping the maxillary sinus (FROMS) is a valid indicator of OAC probability,” wrote the authors, led by M.M. Bakacak of the University of Amsterdam Academic Center for Dentistry in the Netherlands (Clin Oral Investig, April 23, 2025, Vol. 29, 263).
The study involved adult patients referred by general dentists for the extraction of fully erupted maxillary first or second molars between January 2016 and July 2021. A total of 2,340 extractions were performed during this period. OAC was diagnosed immediately after extraction using methods such as visual inspection for sinus exposure and gentle probing of the socket.
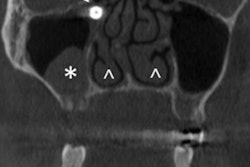
Panoramic radiographs (PANs) from the OAC cases and 100 control cases were analyzed. Researchers identified the sinus floor contour and measured root overlap with the sinus, including the length of the root projected over and outside the maxillary sinus, they wrote.
The FROMS was categorized in diagnostic classes, including A (no overlap), B (0.1% to 25% overlap), C (25.1% to 50% overlap) and D (> 50% overlap). Descriptive statistics were applied to determine the overall OAC rate and the OAC rates for individual tooth types, including the first premolar (P1), second premolar (P2), first molar (M1), and second molar (M2).
A significant association was found between diagnostic classes and the occurrence of OAC, with a chi-square test result of χ² = 42.90, df = 3, and p < 0.0001. The risk of OAC increased across the diagnostic classes with 1% in class A, 3.3% in B, 10.1% in C, and 17.7% in D, they wrote.
By tooth type, the OAC rates were P1 = 1.8%, P2 = 3.6%, M1 = 7%, and M2 = 3.1%, with M1 showing a significantly higher rate compared to P2 (p = 0.039), while differences among the other teeth were not statistically significant. Regression analysis confirmed a significant association between diagnostic class and OAC risk, with odds ratios of one for A, 3.9 for B (p = 0.007), 14.3 for C (p < 0.001), and 25.8 for D (p < 0.001).
However, the study had limitations, including the exclusion of third molars, as third-molar removal is commonly associated with OAC, the authors added.
“The probability of occurrence of OAC following removal of maxillary (pre-)molars can be predicted by determining the fraction of the root overlapping the maxillary sinus on a panoramic radiograph,” they concluded.