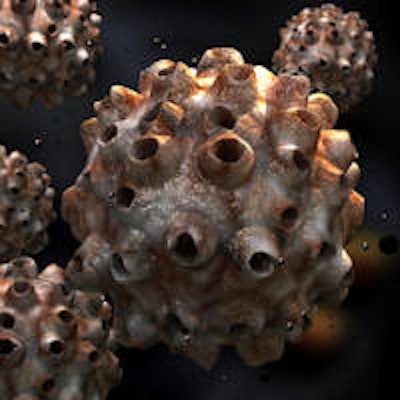
Patients with human papillomavirus (HPV)-positive oropharyngeal cancer have significantly higher rates of complete response after chemoradiation therapy and may avoid neck surgery, according to a study presented at the recent American Society of Radiation Oncology (ASTRO) meeting in San Francisco.
"For patients that achieve a complete response, neck surgery is probably unnecessary," stated lead study author Thomas J. Galloway, MD, an attending physician and the director of clinical research at the Fox Chase Cancer Center, in a statement.
 Thomas J. Galloway, MD
Thomas J. Galloway, MDAfter radiation and chemotherapy to remove tumors from the tonsils or back of the tongue, many head and neck cancer patients still have persistent lumps in their neck, although perhaps smaller than when they were first diagnosed, the study authors noted.
"The question is: Do we need to remove those lumps, as well, or can we just let them dissolve on their own?" Dr. Galloway pointed out.
For this study, he and his colleagues reviewed the medical records of 396 patients whose oropharyngeal tumors had spread to at least one lymph node. Within 180 days after completing radiation therapy, 146 patients had neck surgery. For 99 patients, their records indicated whether or not their tumors were likely triggered by HPV.
Studies show that HPV-positive patients often respond better to treatment for their oropharyngeal tumors than HPV-negative patients. The researchers found the same trend in their study -- people who tested positive for HPV (measured by HPV type 16) were less likely to have a recurrence of their cancers, regardless of whether or not the tumors had completely disappeared following treatment. Indeed, patients' HPV status was the strongest predictor of whether or not they were alive at the conclusion of the study.
“For patients that achieve a complete response, neck surgery is probably unnecessary.”
Among the patients who underwent neck surgery, any lingering bumps were more likely to be benign if patients were infected with HPV. "The bump might have become a permanent scar, or in some cases, it would have eventually disappeared," Dr. Galloway noted.
Currently, it is not routine to consider a patients' HPV status before deciding on neck surgery, which can cause problems in the shoulder and neck, including swallowing. But the study's findings suggest that surgeons should consider HPV status.
"There's good reason to avoid neck surgery if we can," Dr. Galloway stated.
The study was supported by a Radiation Therapy Oncology Group and Community Clinical Oncology Program grant from the National Cancer Institute.



















