A neck mass and sore throat appear to be the initial symptoms in patients with oropharyngeal squamous cell carcinoma (OPSCC), and the symptoms seem to be associated with the human papillomavirus (HPV) status of the tumors, according to a new study in JAMA Otolaryngology -- Head & Neck Surgery (March 20, 2014).
While the incidence of head and neck cancer has been steadily declining, the rates of OPSCC are steadily increasing, a phenomenon explained by the rise in HPV-positive OPSCC. HPV-positive OPSCC tends to affect younger, nonsmoking men and patients with more extensive sexual history.
About 8,400 Americans are diagnosed annually with HPV-related oropharyngeal cancer, according to the U.S. Centers for Disease Control and Prevention. And studies show that patients with HPV-positive OPSCC have a more favorable prognosis and quality of life than those with HPV-negative OSPCC.
This new small, retrospective study is the first to report the most common initial symptoms in OPSCC and illustrates the differences in clinical presentation between HPV-positive and HPV-negative OPSCC, according to South Carolina researchers.
For the study, they analyzed 88 patients with newly diagnosed, previously untreated OPSCC with known HPV tumor status who had been evaluated at the Head and Neck Tumor Center Multidisciplinary Clinic at the Medical University of South Carolina, Charleston, between January 2008 and May 2013.
OPSCC is often diagnosed at an advanced stage, likely owing to the prolonged asymptomatic phase of these tumors. Only 12 of the patients with OPSCC (14%) were diagnosed at an early stage, while 76 (86%) were diagnosed at advanced stages. Of the total 88 patients included in the study, 71 (81%) were HPV-positive and 17 (19%) were HPV-negative.
The HPV-positive group had a higher percentage of whites than nonwhites (93% versus 47%, respectively) compared with prior studies. However, this study detected no statistically significant age difference between HPV-positive and HPV-negative patients with OPSCC (59 versus 60 years, respectively).
Patients who were HPV-negative were more likely to present without nodal disease (N0), compared with HPV-positive patients (35% versus 17%, respectively). Furthermore, HPV-positive patients were more likely to present with T1 disease than HPV-negative patients (24% versus 6%, respectively).
In the study's HPV-positive group, the extent of nodal disease and initial noticeable symptom of neck mass may relate to the current theory of the pathophysiologic characteristics of HPV-positive cancer, the researchers said. HPV typically infects the crypts of the lingual and palatine tonsils.
These crypts are lined with reticulated epithelium composed of an interrupted basal cell layer and basement membrane. This structure facilitates passage of antigens, lymphocytes, and antigen-presenting cells for defense of pathogens entering the upper aerodigestive tract. Consequently, HPV has a direct passage to bind to the heparin sulfate modalities of the basement membrane and infect nearby basal cells, according to the study authors.
Tumor characteristics and results
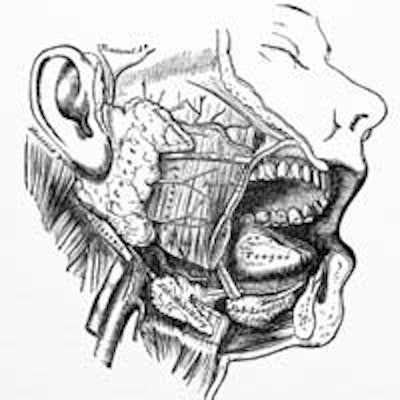
Overall, the study patients' primary tumors were located in the tonsillar complex (46 tumors, 52%), base of tongue (34, 39%), soft palate (6, 7%), and the posterior pharynx (2, 2%). In the HPV-positive group, the location encompassed the tonsillar complex (41 tumors, 58%), base of tongue (26, 37%), soft palate (4, 6%), and none in the posterior pharynx. In the HPV-negative group, the location encompassed the base of tongue (8 tumors, 47%), tonsillar complex (5, 29%), soft palate (2, 12%), and posterior pharynx (2, 12%).
“With the rapidly increasing incidence in OPSCC, it may be important ... to encourage ... dental healthcare professionals to have a high index of suspicion in patients with symptoms suggestive of OPSCC.”
According to HPV tumor status, neck mass was significantly more common in patients with HPV-positive OPSCC versus HPV-negative OPSCC (51% versus 18%, respectively; p = 0.02). Sore throat was more common in HPV-negative OPSCC versus HPV-positive OPCSS (53% versus 28%; p = 0.09). Although less common initial complaints, dysphagia and odynophagia were significantly more associated with HPV-negative OPSCC versus HPV-positive OPSCC (41% versus 10%; p = 0.005; and 24% versus 6%; p = 0.04, respectively).
In addition, the researchers used a Spearman rank correlation test to further analyze symptoms associated with HPV positivity, and found a positive correlation of neck mass with HPV-positive OPSCC (ρ = 0.263; p = 0.01), while sore throat, dysphagia, odynophagia, bleeding, and weight loss were less likely to present as HPV-positive patients' initial symptoms.
A recent study (American Journal of Neuroradiology, October 2013, Vol. 34:10, pp. 2005-2009) showed that HPV-negative tumors were more likely to show radiographical evidence of invasion into adjacent muscle (26% versus 6%; p = 0.01), perhaps correlating with symptoms of HPV-negative tumors that seem to be associated with the primary tumor site in this study, the researchers said.
In this study, symptoms of primary tumor invasion (sore throat, dysphagia, odynophagia, bleeding, weight loss) were associated with HPV-negative tumors.
With the significantly better survival rate in HPV-positive OPSCC, current trials are investigating "deintensification" strategies that reduce radiation and/or chemotherapy therapeutic regimens to decrease morbidity associated with multimodality therapy, the study authors noted.
Conclusion
The most common initial symptoms of OPSCC were neck mass (39) in patients and sore throat (29) in patients. More HPV-positive patients noticed a neck mass as an initial sign, while HPV-negative patients had pain symptoms related to the primary tumor site, including sore throat and uncomfortable or painful swallowing.
A majority of the group (81%) had HPV-positive OPSCC, and for them the most common first symptom was a lump in the neck. Half of those patients had a neck mass, compared with only 18% of patients with HPV-negative cancer.
The differences in clinical presentation between HPV-positive and HPV-negative OPSCC may better support the ongoing theory of how HPV-positive OPSCC tends to originate in the tonsillar crypts resulting in early cervical metastasis, and that HPV-negative OPSCC is more likely to be locally invasive correlating with initial symptoms at the primary tumor site, the study authors concluded.
"With the rapidly increasing incidence in OPSCC, it may be important to consider education of the general public about the early symptoms of OPSCC and to encourage primary care providers and dental health care professionals to have a high index of suspicion in patients with symptoms suggestive of OPSCC," they concluded.