In restorative dentistry, the preservation of natural tooth structure remains a primary objective, aligned with the principles of minimally invasive dentistry. This case study highlights the successful restoration of a cracked posterior tooth using a full-coverage zirconia crown and the immediate dentin sealing (IDS) technique.
By employing evidence-based protocols, advanced materials, and a meticulous clinical approach, the clinician delivered a durable, functional, and aesthetic solution that addressed the patient's concerns while promoting long-term oral health.
Case presentation
A 55-year-old man presented with pain upon biting and cold sensitivity along the gingival margin of tooth #4 (Figure 1). The patient reported taking medication for high blood pressure and experiencing job-related and personal stress, which contributed to his bruxism habit. He had been wearing a nightguard for the past five years to manage the effects of grinding.
 Figure 1.
Figure 1.
Diagnosis and treatment planning
A comprehensive clinical evaluation was performed, including bitewing and periapical radiographs, intraoral photographs, periodontal probing, and an occlusal assessment. Periodontal probing depths ranged from 2 mm to 3 mm, with gingival recession noted.
The existing mesio-occluso-distal (MOD) amalgam restoration on tooth #4 exhibited leakage and recurring decay, as evidenced by radiographic findings. Cold sensitivity that did not linger longer than five seconds was confirmed on the cervical margin of tooth #4, and the heat and percussion tests were negative.
Adjacent teeth #3 and #5 also displayed failing amalgam restorations. The Tooth Sleuth device identified a cracked buccal cusp on tooth #4, and cervical abfractions were observed on the posterior teeth.
After a thorough assessment, two primary treatment options were discussed with the patient:
- A conservative onlay preparation with a separate class V composite restoration to maintain the tooth's ideal compression form
- A full-coverage crown with IDS
The patient, understanding the implications of each approach, elected to proceed with the full-coverage crown with IDS.
Treatment process
After administering local anesthesia and placing a rubber dam, the existing amalgam restoration was removed and the fracture of the buccal cusp was addressed through controlled reduction. One challenge encountered during the treatment process was the presence of deep caries.
To address this issue, the clinician followed the Fusayama concept of selective caries removal, a well-established protocol from the 1980s. Caries Detector dye guided the removal of infected caries, and the tooth was prepared for a Katana Zirconia One crown, following a 1-mm reduction protocol (Figure 2).
 Figure 2.
Figure 2.
The IDS technique was then initiated using the Clearfil SE Protect system. The self-etching primer was applied for 20 seconds, gently air-dried, and followed by the application of the SE Protect bonding agent, which was light cured for 10 seconds (Figure 3).
 Figure 3.
Figure 3.
To insulate and protect the pulp in areas of deep decay, a 0.5-mm layer of Clearfil Majesty Flow flowable composite was placed and light cured for 20 seconds. Subsequently, Clearfil AP-X Composite was incrementally placed and cured in 1-mm layers in areas where tooth structure had been removed, ensuring a uniform ceramic thickness for the final restoration.
A digital impression of the prepared tooth was captured using the CEREC Primescan, extending from the contralateral second bicuspid to allow for accurate occlusal registration. The CEREC software's design proposal was refined by adjusting the model axis, the insertion axis, embrasures, marginal ridge height, fissure height, and proximal contacts, ensuring an ideal occlusal relationship.
The material selected for the final restoration was the Katana Zirconia One Multilayered Block in shade A2, chosen for its exceptional aesthetics, tissue reattachment properties, and superior translucency index among zirconia materials. The restoration was milled using the CEREC MC XL in approximately 15 minutes.
After milling, the sprue was removed, and the restoration underwent prepolishing to eliminate milling scratches and demarcations (Figure 4). It was then sintered in the CEREC SpeedFire oven for approximately 18 minutes.
 Figure 4.
Figure 4.
The try-in phase involved assessing the marginal integrity, verifying passive proximal contacts, and evaluating the occlusion. The restoration was then polished and glazed using Cerabien CZR glaze after microetching the surface.
For cementation, the intaglio surface of the restoration was cleaned with Katana Cleaner and microetched with 50-μm aluminum oxide particles at 32 PSI, followed by ultrasonic cleaning in ethanol (Figure 5).
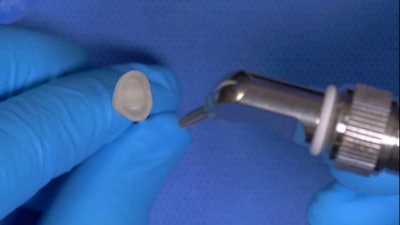 Figure 5.
Figure 5.
The prepared tooth was isolated with a rubber dam, and phosphoric acid was applied to the preparation for 10 seconds to etch the enamel followed by rinsing to clean the surface. Next, Clearfil Universal Bond Quick adhesive was applied for five seconds and gently air-dried.
Panavia SA Cement Universal, containing 10-methacryloyloxidecyl dihydrogen phosphate (MDP) monomer for enhancing the bond to zirconia, was used for the final cementation. After seating the restoration, tack curing was performed at each embrasure for three seconds followed by the removal of excess cement and flossing to clear proximal contacts.
Final light curing was carried out for 10 seconds on each surface. Occlusal adjustments were not required in this case, and a final verification radiograph was taken.
Treatment outcome and follow-up
 Figure 6.
Figure 6.
The treatment met the patient's expectations (Figure 6), alleviating discomfort during chewing and eliminating cold sensitivity, enabling the patient to enjoy cold foods and beverages without discomfort. Since completing the treatment, the patient's oral health has improved. The man was referred for a sleep study evaluation to address bruxism, and adjacent teeth are being restored as needed. Regular hygiene visits were recommended to the patient for maintenance and monitoring.
Dr. Greg Campbell graduated from the University of Southern California School of Dentistry and completed advanced training in Cosmetic Dentistry at UCLA. He is an active member of several dental associations and holds dual bachelor's degrees from Northern Arizona University. Campbell is an expert in advanced adhesion techniques and helps dentists elevate their practice. He lectures and trains dentists on integrating CAD/CAM; mastering inlays, onlays, crowns, and implant crowns; as well as anterior aesthetics like veneers and crowns. He is also skilled in chairside patient-specific implant abutments and crowns.
The comments and observations expressed herein do not necessarily reflect the opinions of DrBicuspid.com, nor should they be construed as an endorsement or admonishment of any particular idea, vendor, or organization.