Imaging assisted in the treatment of a man's third molar that had fused with a supernumerary tooth, according to a case report published July 27 in the American Journal of Case Reports. The man was diagnosed with symptomatic irreversible pulpitis with apical periodontitis.
Fused teeth are a developmental dental anomaly that clinicians need to be aware of, because they show excessive width and irregular anatomy, which can complicate endodontic treatment. In this case, cone-beam computed tomography (CBCT) was used, because it offered a better view of the tooth anatomy, which had an unusual five canals. The patient underwent a root canal without complications, the authors wrote.
"This case report indicates that a proper treatment plan ensures predictable outcomes by the use of all available diagnostic tools," wrote one of the case report's co-authors, Dr. Waleed Almutairi of Qassim University in Saudi Arabia.
A 26-year-old man with severe pain
An otherwise healthy man with good oral hygiene presented at the college's endodontics department after experiencing two days of severe spontaneous pain on the right side of his lower jaw. A dental exam revealed a large tilted, irregular third molar that was fused with the fourth molar. It was tender to the touch and caused pain when cold stimulus was applied. The exam suggested a diagnosis of symptomatic irreversible pulpitis with symptomatic apical periodontitis, the authors wrote.
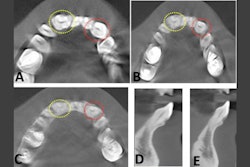
 An intraoral x-ray of the patient's lower right mandibular area revealed a fused third molar and supernumerary tooth with an irregular morphology and a wide mesiodistal width. Radiopacity seen in the furcation area appeared to be the enamel pearl. Licensed by CC BY 4.0.
An intraoral x-ray of the patient's lower right mandibular area revealed a fused third molar and supernumerary tooth with an irregular morphology and a wide mesiodistal width. Radiopacity seen in the furcation area appeared to be the enamel pearl. Licensed by CC BY 4.0.He underwent an intraoral x-ray that showed fused molars with an irregular morphology and a wide mesiodistal width. The 2D view offered by the x-ray made it difficult to identify the demarcation between the pulp chamber of the third molar and the supernumerary tooth. Also, clinicians could not ascertain the root canal configuration of the tooth, according to the report.
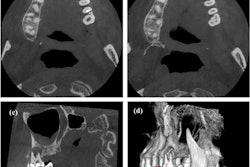
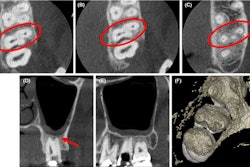
Therefore, the man underwent a CBCT scan, which showed the pulp chamber was continuous, and the tooth had five canals. It had two orifices on the mesial, two in the middle, and one on the distal side.
 Multiple CBCT slices revealed the unilateral fused third with a continuous pulp chamber. The axial view revealed the tooth had five canals.
Multiple CBCT slices revealed the unilateral fused third with a continuous pulp chamber. The axial view revealed the tooth had five canals.After discussing options with the patient, the patient chose to undergo nonsurgical root canal treatment for the fused molar. Once the root canal was completed, an x-ray was taken, and the tooth was restored with a temporary filling. The patient was told to undergo a full coverage restoration at his general dentist within a week, which he completed, they wrote.
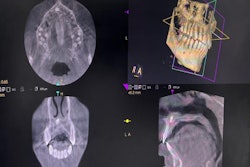
At his six-month follow-up visit, an x-ray showed normal apical tissue with the absence of tenderness on percussion or palpation, as well as no clinical or sinus tract swelling.
 An intraoral x-ray shows (A) a postoperative x-ray of the man's fused third molar with supernumerary tooth and (B) a six-month follow-up x-ray that shows normal bone appearance.
An intraoral x-ray shows (A) a postoperative x-ray of the man's fused third molar with supernumerary tooth and (B) a six-month follow-up x-ray that shows normal bone appearance.Using all available diagnostic tools
Dental fusion is reported in up to 0.2% of permanent dentitions, though the prevalence can be higher in primary teeth. The origin of fused teeth remains unclear; however, trauma and genetics have been suggested as possible etiologies, the authors wrote.
Since fused teeth can have unusual anatomic variations, it is critical that clinicians use imaging to visualize the tooth before treatment. X-rays are essential tools in endodontics, but they don't consistently show the precise anatomy of the root canal system, they wrote.
Furthermore, CBCT must be considered the modality of choice for any dental anomalies, according to a position statement from the American Association of Endodontists and the American Academy of Oral and Maxillofacial Radiology.
"Successful treatment can be predicted when clinicians use a proper treatment plan and utilizing all available diagnostic tools," they wrote.