Two patients experienced strokelike symptoms after hyperextending their necks during dental treatment, according to a case report recently published online in the Neurologist.
The two patients described in the report underwent dental procedures in which clinicians hyperextended their necks for better reach or tooth access. Afterward, they both experienced neurological symptoms and were hospitalized.
Though both patients survived, these cases highlight a "plausible correlation" between their symptoms and the overstretching of their necks during routine dental treatment, said Victor El-Hajj, one of the authors and a third-year medical student at the Karolinska Institute in Stockholm.
These cases aim "to encourage research on this rare complication of neck positioning on dental chairs," El-Hajj and colleagues wrote (Neurologist, January 20, 2022).
Case 1: Vertigo after bridgework
In the first case, a 67-year-old man went to the dentist for bridgework. He had no history of cerebrovascular events but was taking medication for high blood pressure.
For the 45-minute procedure, the man was placed under local anesthesia, and his neck was hyperextended for better reach. Right after the dental work, the man said he was experiencing vertigo and an occipital headache and he couldn't stand up.
Immediately, the patient was transported to a hospital emergency room where he received a neurological consultation. The exam revealed the man had dysmetria, involuntary eye movements, a positive Romberg sign, facial paresis, and trouble swallowing. These symptoms were consistent with lateral medullary syndrome, and magnetic resonance imaging (MRI) and magnetic resonance angiography (MRA) confirmed the diagnosis.
After he was given heparin, the patient improved. Though he still had minor swallowing difficulties and gait instability, the man was discharged after 17 days in the hospital. He continues to take low-dose aspirin and has had no further problems, the authors wrote.
Case 2: Dizziness after an extraction
In the second case, a 64-year-old woman visited the dentist because of an ill-fitting prosthesis. The patient was obese, smoked 30 cigarettes per day for 40 years, and had diabetes.
A clinical exam showed discharging pus and a fistulous tract in her left upper jaw-crest area, and an x-ray revealed an unerupted wisdom tooth in the area. The woman was scheduled to undergo tooth extraction and removal of the fistula tract.
The patient was placed under local anesthesia for the 40-minute procedure. To gain adequate access to the tooth site, her neck was hyperextended. After the procedure, she left the clinic without any symptoms.
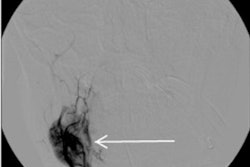
On the day after the procedure, the woman felt dizzy and lost her balance. She was taken to the hospital, where a neurological exam revealed dysmetria, facial paresis, and a bilateral Babinski sign. Though an MRI showed nothing remarkable, MRA revealed congenital hypoplasia of the right vertebral artery.
She was given heparin, and her symptoms were gone after two days. The patient was diagnosed with a transient ischemic attack and prescribed daily low-dose aspirin, according to the authors.
Dentistry's beauty parlor syndrome?
El-Hajj and colleagues believe the two cases are among the first of their kind to be described in dentistry. However, other scenarios that involve people extending their necks for long periods of time have been linked to neurological effects.
In the early 1990s, beauty parlor syndrome, or a hairdresser-related ischemic cerebrovascular event, was first described as a condition in which individuals experience a neurological event due to hyperextending their necks during hair washing.
Though positioning patients in a dental chair is not thought to cause any medical conditions, previous evidence indicates patients may experience malaise, fainting, high blood pressure, and other rare symptoms. The current report shows that routine dental treatment has the potential to cause major neurological events, according to the authors.
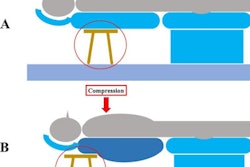
Vertebrobasilar insufficiency and posterior circulation ischemia can occur during hyperextension of the neck, possibly due to the impingement of blood vessels. Risk factors for cerebrovascular diseases, including older age, diabetes, and obesity, may also play a role in these incidents.
Possible precautions
Clinicians should be informed about the potential for this type of acute ischemic attack and be aware of patients with risk factors, the authors wrote.
There is not enough information to offer specific preventive recommendations; however, simple steps could be taken to lower the risk of complications, including asking patients about medical conditions such as high blood pressure, diabetes, and atherosclerosis and lifestyle habits such as smoking.
Additionally, clinicians may want to avoid having patients extend back in chairs for prolonged periods of time and give high-risk patients a break every 10 to 12 minutes, the authors suggested.
Finally, after lengthy dental treatment, patients should be monitored for symptoms like headache, neckache, and blurred vision.
"Obtaining immediate medical care in cases of ischemic attacks is imperative as any delay might result in severe irreversible damage," El-Haff and colleagues wrote.