Many people have felt the jolting sensation of feeling a sharp pain in a tooth after drinking cold beverages. If the pain is caused by pulpitis, the treatment often requires a root canal procedure to remove the damaged pulp.
 Radi Masri, BDS, PhD, associate professor, University of Maryland School of Dentistry Department of Endodontics, Prosthodontics and Operative Dentistry, is developing a technique to deliver medication directly into the center of a tooth. Image courtesy of University of Maryland School of Dentistry.
Radi Masri, BDS, PhD, associate professor, University of Maryland School of Dentistry Department of Endodontics, Prosthodontics and Operative Dentistry, is developing a technique to deliver medication directly into the center of a tooth. Image courtesy of University of Maryland School of Dentistry.Now, research being conducted at the University of Maryland School of Dentistry could provide dentists with a much less invasive treatment for pulpitis. Radi Masri, BDS, PhD, an associate professor in the department of endodontics, prosthodontics, and operative dentistry, is developing a new, patent-pending technique to deliver medication directly to the center of a tooth.
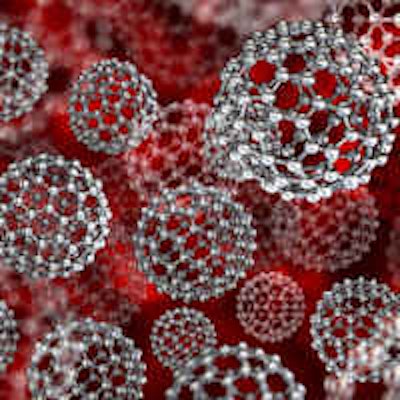
Dr. Masri and his collaborator, Didier Depireux, PhD, an associate research scientist at the A. James Clark School of Engineering at the University of Maryland, College Park, recently received a two-year, $450,000 grant from the National Institute of Dental and Craniofacial Research for their project, "Magnetic Delivery of Therapeutic Nanoparticles to the Dental Pulp."
The study uses strong magnetic fields to move microscopic particles through the tooth's dentin and into the pulp.
"When you have a cavity, usually the enamel has been damaged and the dentin is exposed, so when you eat or drink, it will stimulate the fluid within the dentinal tubules and cause pain," Dr. Masri explained in a press release.
He envisions using the tubules -- microscopic channels that travel through the dentin into the tooth pulp -- as a vehicle to deliver medication that could reduce inflammation or treat infection. The technique would attach medication to nanoparticles. By creating the nanoparticles out of a magnetic substance, such as iron, the researchers can use a magnetic field to push those particles, and the attached medication, through the tubules and into the pulp.
“We have been treating pulpal inflammation the same way for decades. This is a contemporary approach to an age-old problem.”
Drs. Masri and Depireux have designed a system of magnetic arrays that are effective for upper or lower teeth. By manipulating a series of cube-shaped magnets, they can control the magnetic field so the nanoparticles are pulled through the tubules into the tooth pulp. Delivering steroid medication using these magnetic nanoparticles could treat inflammation in the pulp. An antibiotic could be delivered to reduce the infection, or a local anesthetic could be used to anesthetize a tooth.
Dr. Masri's research has shown that, even though the nanoparticles are tiny, they are able to deliver a large enough dose for medications to be effective. He is currently conducting studies on extracted human teeth to determine the optimal size for the nanoparticles and the most effective biocompatible coating. By covering the particles with a biocompatible substance -- starch for example -- the body's immune system won't attack the nanoparticles, he explained.
Dr. Masri hopes the grant will allow him to conduct enough preliminary studies to eventually move the project into human trials. Testing in live patients will allow him to determine if the procedure actually reduces pain.
He is encouraged about the implications the project holds for the future of dental care. "We have been treating pulpal inflammation the same way for decades," Dr. Masri stated. "This is a contemporary approach to an age-old problem."