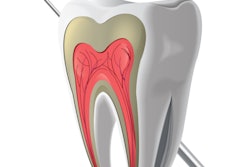
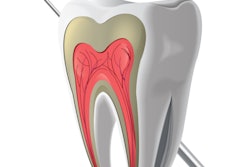
Biomarkers found in pulp have the potential to improve the accuracy of the diagnosis and treatment of pulpitis, according to a new study. This may be a step toward development of a chairside test to alert patients and practitioners to the presence of inflammation.
The researchers examined published studies to determine if measurements of various biomarkers in irreversible pulpitis were different compared with nondiseased conditions. Their results were published in PLOS One (November 29, 2016).
"The main current challenges in the clinical application of biomarkers lie in the identification of biomarkers or biomarker subsets that reliably correlate with pulpal inflammation, the improvement of sample collection (substrate and protein yields), and their analysis (interference of the biomarkers with inflammation of other than pulpal origins)," wrote Dan-Krister Rechenberg, DMD, and colleagues. "If these hurdles can be overcome, a more accurate pulpal diagnosis and more predictable vital pulp treatment regime may create better clinical outcomes."
Dr. Rechenberg is a senior assistant in endodontology at the University of Zurich Center of Dental Medicine in Switzerland. The study co-authors were Johnah Galicia, DDS, an assistant professor of endodontics, and Ove Peters, DMD, PhD, co-chair of the department of endodontics, at the University of the Pacific Arthur A. Dugoni School of Dentistry in San Francisco.
Combing the literature
Currently, no diagnostic procedures or tests reliably diagnose the inflammatory status of pulp. The authors noted that this is unfortunate, as decision-making for appropriate treatment, such as differentiating between the need for vital pulp therapy and root canal treatment, depends on accurate diagnosis.
While the role of cytokines, proteases, inflammatory mediators, growth factors, antimicrobial peptides, among others in the body's response to pulpitis is well-documented, these factors may serve as biomarkers that can be used to diagnose or stage pulpal inflammation. The importance of identifying these biomarkers warrants additional study, as well as a critical or systematic review and analysis of published reports, according to the study authors.
Therefore, they conducted a systematic review of biological markers for pulpal inflammation, including electronic databases and other sources published through February 2015.
They found 57 eligible studies that clinically or histologically differentiated between a healthy and irreversibly inflamed pulp in permanent human teeth and analyzed interstitial/dentinal liquor, gingival crevicular fluid, pulpal tissue, dentin fluid, or apical blood for the presence of a biological marker. The researchers defined a biological marker as a measurable and quantifiable biological molecule that theoretically can be present in those substrates and might serve as an indicator for a healthy or diseased pulp.
“The ultimate goal should then be to develop an inexpensive chairside test for noninvasive molecular pulp diagnostics.”
Fifty of the studies analyzed pulp tissue for the presence of a biomarker collected either via pulpectomy or tooth extraction and fracturing, or a combination of both. The remaining seven studies analyzed substrates other than pulp tissue: pulpal blood, peripheral blood serum, dentinal fluid, or extracellular pulpal fluid. Of the studies analyzing pulp tissue, 41 used tissue collected from extracted healthy, noncarious permanent, or wisdom teeth as their control.
Among the studies, pulp tissue was assessed for 89 biological markers. Statistically significant differences between irreversible inflamed and healthy pulp were detected for 64 biological markers (71.9%) by at least one study, while 19 of the markers did not show any statistically significant differences between inflammation and health. Six biological markers were not used in the statistical tests. A substrate other than pulp tissue was evaluated for 16 biological markers, with statistically significant differences between irreversible inflammation and healthy tissue detected in 12 of the 16 (75%) by at least one study.
The current study results point to a response by immunocompetent tissues in pulpitis that results in a release of mediators that triggers inflammation to begin the healing process, the authors noted.
The biomarkers were significantly expressed in pulp tissue and also in gingival crevicular fluid that can be collected noninvasively and in dentin fluid that can be analyzed without extirpating the entire pulpal tissue, they reported. Such data could be used to accurately differentiate diseased from healthy pulp tissue, they noted.
Improving diagnosis and outcomes
A limitation of the study was that only two of the 57 studies were designed to investigate potential biomarkers for use in pulpal diagnostics.
However, the current review may provide the impetus for further research exploring factors related to patients (such as age, gender, and systemic condition) and infection (varying composition of the microbiological infection), the authors wrote.
"The ultimate goal should then be to develop an inexpensive chairside test for noninvasive molecular pulp diagnostics," they concluded.