Johns Hopkins researchers have developed blood and saliva tests that can accurately predict the recurrence of oropharyngeal squamous cell carcinoma (OPSCC) linked to human papillomavirus (HPV). Finding HPV DNA in both blood and saliva samples after treatment accurately predicted recurrence 70% of the time in patients.
The researchers investigated the role of HPV type 16 (HPV16) DNA detection as a biomarker for OPSCC disease status. Their findings are outlined in a study in JAMA Otolaryngology -- Head & Neck Surgery (July 31, 2014).
The study is the first and largest so far to determine the feasibility of early detection of HPV16-positive primary cancer and recurrence using the quantitative polymerase chain reaction (PCR) technique, the researchers noted. But they added that the study was limited by the small number of patients.
Participants
While the overall incidence of head and neck cancer is decreasing in the U.S., recognized cases of oropharyngeal squamous cell carcinoma are on the rise. About 70% of an estimated 30,000 oropharyngeal cancer cases in the U.S. annually are attributed to HPV. Studies show improved overall survival in HPV16-positive OPSCC patients versus HPV16-negative patients, the authors wrote.
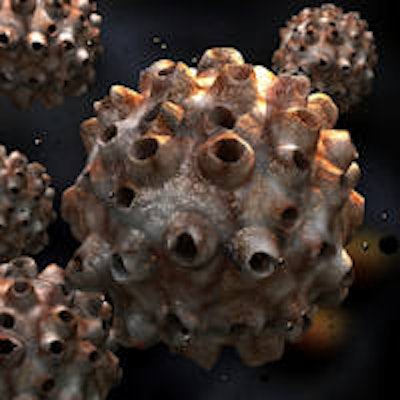
 Electron micrograph of a negatively stained HPV. Image courtesy of the Laboratory of Tumor Virus Biology, National Institutes of Health.
Electron micrograph of a negatively stained HPV. Image courtesy of the Laboratory of Tumor Virus Biology, National Institutes of Health.Patients with HPV-associated oropharyngeal cancers are generally examined every one to three months in the first year after diagnosis. Recurrences are often found when patients report ulcers, pain, or lumps in the neck. The study authors noted that imaging tests are often unreliable in detecting cancer recurrence earlier, and the location of oropharyngeal cancers -- in the tonsils, throat, and base of the tongue -- make it difficult to see these lesions.
For this study, researchers evaluated 93 Maryland patients (81 patients had HPV-positive tumors) with OPSCC who were treated with surgery, radiation alone, or combined chemotherapy and radiation from 1999 to 2010 at the Johns Hopkins Hospital or Greater Baltimore Medical Center. The patients were nonsmokers and generally had advanced-stage disease with lymph node metastasis.
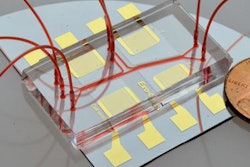
The researchers selected patients with a variety of early- to advanced-stage cancers; none of the patients had distant metastasis. Samples were collected before and after treatment. The plasma and saliva tests were done using the PCR protocol, which amplifies certain portions of DNA and measures its amount.
With a median follow-up time of 49 months, 19 of 93 patients (20%) developed recurrence after completing treatment. Of these 19, 14 patients had HPV16-positive tumors and five patients had HPV16-negative tumors.
Results
Before treatment, sensitivity for the salivary-based screening test was 52.8%, which improved to 67.3% using plasma-based screening, the researchers found. Sensitivity rose to 76.1% using both plasma- and saliva-based screening tests.
“Until now, there has been no reliable biological way to identify which patients are at higher risk for recurrence, so these tests should greatly help do so.”
After treatment, the sensitivity and specificity of salivary HPV16 status in HPV16-positive tumors in predicting recurrence within three years were 18.8% and 96.6%, respectively. The sensitivity and specificity of surveillance plasma HPV16 status were 55.1% and 95.6%, respectively. When combining post-treatment saliva and plasma samples, the presence of HPV16 DNA was 90.7% specific and 69.5% sensitive in predicting locoregional or metastatic recurrence within three years in the study group.
Both HPV DNA positivity in post-treatment saliva and plasma in patients with HPV16 positive tumors were significantly associated with worse recurrence-free survival, the study authors noted. Eight patients (10%) with HPV-positive tumors died.
The sensitivity achieved by combining the surveillance saliva and plasma HPV16 status is better when compared with the sensitivity of a three-month post-treatment PET/CT, the researchers noted.
Conclusion
Quantitative PCR detection of HPV DNA in post-treatment surveillance saliva and plasma samples can function as a valuable prognostic biomarker of recurrence-free survival and overall survival in patients with HPV-positive OPSCC, the study authors concluded.
"There is a window of opportunity in the year after initial therapy to take an aggressive approach to spotting recurrences and intensively addressing them while they are still highly treatable," study co-author Joseph Califano III, MD, said in a statement. Dr. Califano is a professor of otolaryngology -- head and neck surgery, a member of the Johns Hopkins Kimmel Cancer Center, and the medical director of the Milton J. Dance Jr. Head and Neck Center at the Greater Baltimore Medical Center. "Until now, there has been no reliable biological way to identify which patients are at higher risk for recurrence, so these tests should greatly help do so."