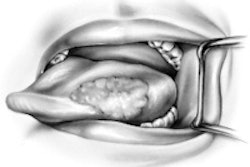
Wider surgical margins for early tongue tumors may reduce local recurrence and improve survival for most early-stage (T1 or T2) oral tongue squamous cell carcinoma (SCC) tumors, according to a new study in the Journal of Laryngology & Otology.
Oral tongue SCC is usually treated with initial surgical resection with or without post-operative chemo- and radiotherapy. Regional recurrences occur in approximately one in four patients with T1 or T2 oral tongue SCC, justifying aggressive treatment, according to the study authors from the University of Melbourne (JLO, March 2012, Vol. 126:3, pp. 289-294).
“We feel that wider surgical margins may be justified, being the only prognostic factor that surgeons have the ability to improve.”
Among the most important histological factors that impact the prognosis for early oral cancer are lymph node metastases, extracapsular extension, and close or involved surgical margins, they noted.
"Although other factors have an impact on adjuvant treatment, surgical margins is the only factor that may be improved by the surgeon," they wrote.
Traditionally, a 1-cm margin is taken in all planes around a macroscopic or palpable oral tongue SCC, the study authors noted. Pathologists and clinicians have agreed to define involved margins as less than 1 mm and close margins as 5 mm or less, while margins greater than 5 mm are designated as clear.
However, mucosal margins shrink by approximately 30% to 50% with formalin fixation and slide preparation. This results in a final pathological margin of approximately 5 mm where the surgeon measured 1 cm, leaving little room for error.
Statistically significant findings
For this study, the research team set out to determine the site of closest margins for previously untreated early oral SCC cases from 2000 to 2009 at Royal Melbourne Hospital. The median age at diagnosis was 63.
Through a retrospective chart review, the researchers identified 68 T1 tumors and 13 T2 tumors, with a median follow up of 38 months. Sites of close and involved margins were reviewed histologically.
Slides were categorized as clear if the margin was more than 5 mm (n = 24), close if the margin was 1.1 to 5 mm (n = 44), and involved if the margin was less than 1 mm (n = 10).
The site of close and involved margins was classified according to its quadrant, i.e. medial, lateral, anterior or posterior. Close and involved margins were also designated as deep (more than 3 mm from the cut mucosal edge) or mucosal (less than 3 mm from the mucosal edge or on the actual mucosa).
Other prognostic variables included depth of invasion, tumor differentiation, maximum diameter, lymphovascular invasion, perineural invasion, pathological cervical nodes, and extracapsular extension.
The researchers found clear margins in 24 patients (30.8%), close margins in 44 patients (56.4%), and involved margins in 10 patients (12.8%). There was a non-significant trend toward deeper tumors having more involved margins (p = 0.18). Clear or close margins were just as likely to be achieved in T1 cases (90%) as in T2 cases (82%) and node-negative (100%) and node-positive cases (82%).
Perineural or lymphovascular invasion was seen equally in cases with involved margins (20%) and cases with clear or close margins (21%).
Patients with deeper tumors were more likely to undergo neck dissection for the N0 neck than patients with thin tumors (p = 0.02). Four patients (22%) with a tumor depth of 2.1 to 4 mm had a prophylactic neck dissection, as did 15 patients (58%) with a tumor depth of 4.1 to 7 mm.
A majority of the tumors had the closest margin at or near the mucosal edge (59%) rather than on the deep surface (41%, p = 0.22), the study found.
1-cm margins 'inadequate'
Local recurrence occurred in 22 patients (28%) at a median of 12 months. Five of the 10 patients (50%) with involved margins developed local recurrence, the study found. Nine (21%) of the 43 patients with close margins had local recurrence, compared with eight (33%) of the 24 patients with clear margins (p = 0.10).
The study found that involved surgical margins had a trend to worse local recurrence (p = 0.10) and significantly worse survival (p = 0.002). Over the last 10 years at the hospital, 14% of patients had involved margins and 55% had close margins, the researchers noted.
"Consequently, we feel that wider surgical margins may be justified, being the only prognostic factor that surgeons have the ability to improve," the researchers wrote.
Histological clear margins may be one of the few prognostic factors on which good surgery can have an impact, they added. Wider margins, however, may have an impact on functional outcomes and significantly affect quality of life.
"This study's findings support the hypothesis that wider surgical margins may be appropriate for most T1and T2 oral tongue SCC tumors, with the aim of reducing local recurrence and thereby improving survival," the study authors concluded. "The historically accepted 1-cm margin around macroscopic and palpable oral tumors seems to provide inadequate pathological results."