Tumor thickness and lymph node metastasis are independent predictors of survival in patients with squamous cell carcinoma of the tongue, according to a new study in the Journal of Oral and Maxillofacial Surgery (July 2013, Vol. 71:7, pp. 1283-1290).
Oral tongue squamous cell carcinoma (OTSCC) is the most common cancer diagnosed in the oral cavity, comprising 25% to 40% of oral carcinomas, noted the Turkish researchers.
The most important prognostic factor is when nodal metastasis is present in the neck, the researchers noted. Tumor, node and metastasis (TNM) stage, grade, and tumor depth also are important factors in predicting the course of disease. The clinicopathologic prognostic factors of tongue squamous cell carcinoma are important for clinicians for determining the aggressiveness of the disease and the appropriate postoperative therapies.
The researchers reviewed the files of 138 patients who had been treated for tongue squamous cell carcinoma at Hacettepe University Hospital from 1980 to 2010. There were no known risk factors in 49.3% of patients; 33.3% of patients were smokers and did not consume alcohol, and 16.7% smoked and consumed alcohol.
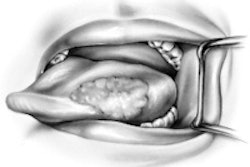
Surgery was the primary treatment modality. All patients underwent partial glossectomy as the initial treatment. Patients who were treated with radiotherapy as the primary treatment modality were excluded. Surgery combined with radiation or chemotherapy was used with 47 patients. Of these, 24 patients received postoperative radiation therapy, and 23 patients with extracapsular spread or positive surgical margins received postoperative chemoradiotherapy.
Survival rates
With a median follow-up period of 23 months for surviving patients, data were available for 138 patients. Nineteen patients (13.8%) had died from tongue cancer, and no patients died from noncancer-related causes.
Five-year overall survival (OAS), disease-specific survival (DSS), and relapse-free survival (RFS) rates for the entire cohort of patients were 81%, 73%, and 71%, respectively. Because this study included patients treated within a 30-year period, survival rates were analyzed according to 10-year periods. From 1980 to 1990, 19 patients were treated for OTSCC, and the OAS and DSS rates were 93% and 75%, respectively. From 1991 through 2000 (n = 26), the OAS and DSS rates were 79% and 73.8%, respectively. From 2001 through 2010 (n = 91), the OAS and DSS rates were 78.9% and 70.6%, respectively. Statistical analysis showed no significant difference in survival rates after comparing these three decades (p > 0.05).
The five-year OAS, DSS, and RFS rates were similar in patients younger than 40 years (90%, 69%, and 64%, respectively) and those older than 40 years (80%, 73%, and 72%, respectively; p > 0.05 for all comparisons).
The OAS, DSS, and RFS rates for patients with risk factors (smoking and alcohol use; n = 70) were 73%, 64%, and 66%, respectively, compared with 89%, 81%, and 76%, respectively, for patients without risk factors (n = 68). The researchers found a significant difference in OAS (p = 0.025) between patients with and those without risk factors. In the study group, 46 patients smoked tobacco and did not consume alcohol. The five-year OAS, DSS, and RFS rates were 76%, 71%, and 72%, respectively, for smokers compared with 88%, 81%, and 76%, respectively for nonsmokers. Although lower survival rates were seen in the smoker group, they found no significant association between smoking and survival rates (p > 0.05).
Twenty-four patients consumed tobacco and alcohol, and there was a significant difference in OAS (p = 0.012) and DSS (p = 0.033) between those who used tobacco and alcohol and those who did not, the study authors noted.
The five-year OAS rate for patients with an early TNM stage was 84%, compared with 74% in patients with an advanced stage. There was no significant difference in OAS between early and advanced stages (p = 0.083). The five-year DSS and RFS rates for patients with an early TNM stage were 77% and 75%, respectively, compared with 62% and 60%, respectively in patients with an advanced stage. There were significant differences in DSS and RFS between early and advanced TNM stages (p = 0.034 and p = 0.027, respectively).
Lymph nodes
Approximately half of tongue cancers present with lymph node involvement, the researchers noted. Lymph node metastasis is a well-known negative prognostic factor for tongue squamous cell carcinoma, which decreases the survival rate by 50%, the researchers noted. This study showed a significant survival advantage for patients with node-negative disease (five-year OAS: 86%).
Patients with uninvolved nodes had significantly better survival rates at five years compared with patients with involved nodes (p = 0.002 for OAS, p < 0.001 for DSS, p = 0.001 for RFS). Also, patients with a single involved lymph node had a better prognosis compared with patients with multiple involved lymph nodes (p = 0.006 for OAS, p = 0.027 for DSS, p = 0.015 for RFS).
For patients with clinical and pathological N0 tumor, the five-year OAS, DSS, and RFS rates were 85%, 79%, and 77%, respectively, and these rates were lower in patients with cN0-pN+ tumor (68%, 54%, and 57%, respectively). Extracapsular spread was identified in 11 of 45 patients (24%) with involved lymph nodes. There was no significant difference in OAS (p = 0.820), DSS (p = 0.804) and RFS (p = 0.204) between patients with and those without extracapsular spread.
The five-year OAS, DSS, and RFS rates were 92%, 89%, and 88%, respectively, for patients with tumor thickness no greater than 8 mm, compared with 70%, 54%, and 52%, respectively for patients with tumor thickness greater than 8 mm. There were significant differences in OAS (p = 0.015), DSS (p = 0.002), and RFS (p = 0.004) between patients with tumor thickness no greater than 8 mm and those with tumor thickness greater than 8 mm.
The researchers found that surgical margin was a prognostic factor that affected DSS and RFS. Tumor thickness greater than 8 mm was the only independent poor prognostic factor that affected OAS in tongue carcinoma. Lymph node metastasis also was associated with a poor prognosis for DSS and RFS, the study authors concluded.