Scientists from the University of Pennsylvania have demonstrated the ability to both prevent periodontitis from developing and halt the progression of the disease once it has developed, according to study in the Journal of Immunology, (December 1, 2012, Vol. 189:11, 5442-5448).
In the study, led by Toshiharu Abe, a postdoctoral researcher in the department of microbiology in Penn's School of Dental Medicine, the researchers impacted periodontitis by blocking a molecular receptor that bacteria normally target to cause the disease in a mouse model.
In previous research, Abe's colleagues showed that Porphyromonas gingivalis, the bacterium responsible for many periodontitis cases, acts to "hijack" a receptor on white blood cells called C5aR. The receptor is part of the complement system, a component of the immune system that helps clear infection but can trigger damaging inflammation if improperly controlled.
By hijacking the receptor, P. gingivalis subverts the complement system and handicaps immune cells, rendering them less able to clear infection from the gum tissue, according to the researchers. As a result, numbers of P. gingivalis and other microbes rise and create severe inflammation. According to a study published last year by the Penn researchers, mice bred to lack C5aR did not develop periodontitis.
Meanwhile, other studies by the Penn group and others have shown that Toll-like receptors (TLRs) -- a set of proteins that also activate immune cell responses -- may act in concert with the complement system. In addition, mice lacking one form of TLR called TLR2 do not develop bone loss associated with periodontitis, just like the C5aR-deficient mice.
In the new study, the Penn team wanted to determine if the synergism seen by other scientists between the complement system and TLRs was also at play in this inflammatory gum disease. To find out, they injected two types of molecules, one that activated C5aR and another that activated TLR2, into the gums of mice.
When only one type of molecule was administered, a moderate inflammatory response was apparent a day later, but when both were injected together, inflammatory molecules increased dramatically -- soaring to levels higher than would have been expected if the effect of activating both receptors was merely additive.
This finding suggested to the scientists that the Toll-like receptor signaling was somehow involved in "cross talk" with the complement system, serving to augment the inflammatory response. They wondered whether blocking just one of these receptors could effectively halt the inflammation that allows P. gingivalis and other bacteria to thrive and cause disease.
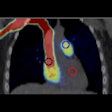
Testing this hypothesis, the researchers synthesized and administered a molecule that blocks the activity of C5aR, to see if it could prevent periodontitis from developing. They gave this receptor "antagonist," known as C5aRA, to mice that were then infected with P. gingivalis. The C5aRA injections were able to stave off inflammation to a large extent, reducing inflammatory molecules by 80% compared with a control and completely stopping bone loss.
And when the mice were given the antagonist two weeks after being infected with P. gingivalis, the treatment was still effective, reducing signs of inflammation by 70% and inhibiting nearly 70% of periodontal bone loss.
Regardless of whether the researchers administered the C5a receptor antagonist before the development of the disease or after it was already in progress, their results showed that they were able to inhibit the disease either in a preventive or a therapeutic mode, they noted.
The results are significant for extending these findings to a potential human treatment, as treatments would most likely be offered to those patients already suffering from gum disease.