A periodontal disease pathogen promotes the activation of immune system cells that can exacerbate the progression of chronic obstructive pulmonary disease (COPD), according to a study recently published in mSystems.
Porphyromonas gingivalis (P. gingivalis) activates gamma delta (γδ) cells and M2 macrophages, which is the immune mechanism that mediates gum disease-promoted COPD progression, the authors wrote.
“Therefore, targeting at periodontitis treatment and the γδ T-M2 immune mechanism might provide a new practical strategy for COPD prevention or control,” wrote the authors, led by Yan Li, PhD, of the West China Hospital of Stomatology at Sichuan University (mSystems, January 12, 2024).
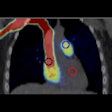
Oral health changes result in an immune imbalance, causing oral immune cells to migrate to the lungs and disrupt the immune balance in lung tissue. Additionally, shifts in oral health can advance lung disease progression by influencing systemic inflammation.
To examine the impact of periodontitis on COPD progression, researchers created the following models: healthy mice, mice with periodontitis only, mice with COPD only, and mice with both COPD and periodontitis. In the process of constructing the periodontitis model, mice were orally infected with P. gingivalis (1 × 109 colony-forming units/mL, 0.2 mL/mice) every other day.
Researchers discovered an elevated abundance of P. gingivalis in COPD lung tissue due to periodontitis. The bacteria traveled, infecting the lung tissue, leading to a noticeable change in the type of bacteria in the lungs. Subsequent flow cytometry and immunofluorescence observations demonstrated that periodontitis facilitated the proliferation of immune cells in the lung tissue.
In mouse lung tissue experiments, the group established the link, demonstrating that P. gingivalis activated the immune cells γδ T cells and M2 macrophages, enhancing their cytokine production associated with exacerbating COPD, they wrote.
However, the study had limitations, including the group imbalance in the number of patients in the state of acute exacerbation, they wrote.
“The results indicated that targeting at periodontitis treatment and the γδ T-M2 immune mechanism might provide a new practical strategy for COPD prevention or control,” Li et al wrote.