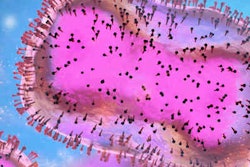
Over recent months, mpox has reemerged in more than 88 countries. Researchers are encouraging dentists to implement droplet infection control measures, patient isolation, and referral during local outbreaks.
Mpox is a highly contagious infectious disease marked by a rash that eventually scabs over and heals. The World Health Organization (WHO) declared the current mpox outbreak as a public health emergency of international concern.
Researchers reviewed the salient features of mpox and its possible implications for dentistry in an article published on August 4 in the International Dental Journal.
"Dental care workers should note that premonitory signs of the disease usually appear on the oral mucosa as macules and ulcers prior to the characteristic skin lesions," wrote the study authors, led by Dr. Lakshman Samaranayake of the University of Hong Kong in China.
What providers should know about mpox
Mpox was first documented in humans in the 1970s, and while infrequent outbreaks have been reported in many countries, recently mpox has rapidly emerged in cities among individuals who are not connected with nor who have traveled outside of the U.S. Several hypotheses have been presented to explain the current outbreak.
"The most favored is the general decline in the population immunity to smallpox and similar Orthopoxvirus diseases, as the smallpox vaccination programme was discontinued 30 years ago," wrote the article's authors.
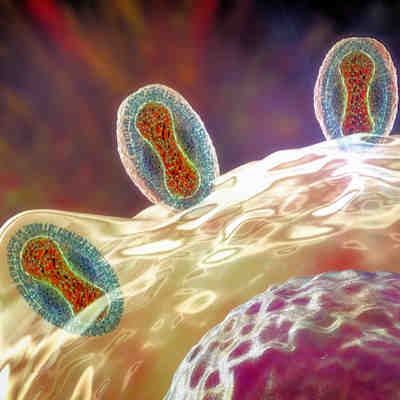
Early symptoms of mpox include fever, headache, muscle aches, chills, fatigue, and generalized lymph node swelling. Mucosal lesions in the mouth are a crucial early sign of mpox.
Patients infected with the mpox virus develop characteristic skin lesions on the face and extremities. The rash undergoes the typical macular, papular, vesicular, and blister stages. Finally, the blisters break and form a scab that eventually falls off.
Cases of mpox are usually mild, with a recovery period of a few weeks. However, mortality rates differ depending on the viral type. Children, young adults, and those who are immunocompromised have a higher mortality rate.
Implications for dental practice
Using data from the current scientific literature, the researchers analyzed mpox's etiology, transmission modes, signs and symptoms, diagnosis, and management, including the risk of its occupational transmission in dental settings. Of interest to the dental field is that the primary lesions caused by mpox originate in the oropharynx before manifesting on the skin. Oral ulcers have been reported in almost one-quarter (23.5%) of patients with the virus.
In disease-endemic regions, dental professionals may be the first to detect the initial symptoms of mpox. The researchers urge dental healthcare workers to maintain a high degree of suspicion, especially when examining patients with lymphadenopathy.
In light of the continual outbreak, clinicians evaluating patients experiencing a fever and rash should consider mpox, especially if lymphadenopathy is also present. The recommended test for identifying the mpox virus according to the WHO is the real-time polymerase chain reaction (PCR) test. PCR tests are generally available at state laboratories for public health. Commercial tests are not currently available.
Transmission in dental care settings can be prevented by taking standard, contact, and droplet infection control precautions when treating patients with the symptoms of mpox. Additionally, due to the potential risk of airborne transmission, airborne precautions should be taken, and N95 masks should be worn by attending dental personnel. The patient should be treated in isolation, and precautions should be taken to minimize exposure to surrounding individuals.
Principal preventive measures against infection with the mpox virus are provided by the UK Health Security Agency. The agency's recommendations include the following:
- Elective dental treatment in patients with suspected or confirmed mpox should be postponed until the patient is no longer infectious.
- If treatment is essential, patients should be treated in isolation.
- Pregnant persons and severely immunocompromised persons should not provide care for patients with suspected or confirmed mpox.
- Standard, contact, and droplet infection control precautions should be taken, including wearing N95 masks, filtering facepiece (FFP3) respirators, fluid-resistant attire, and eye protection.
- Proper hand hygiene should be performed after contact with infected individuals.
- Avoid touching materials that have come into contact with a patient with suspected or confirmed mpox.
- Patient care equipment should be precleaned prior to sterilization.
- Handle linens, hospital gowns, towels, and other fabrics carefully.
"Implementing standard, contact, and droplet infection control measures, patient isolation, and referral are important, particularly during a local outbreak," Samaranayake and colleagues concluded.