A healthy 52-year-old woman died after developing a pyopneumothorax, a collection of pus and air between the lung and the chest wall, caused by a typically benign mouth bacterium. The case report was published on October 23 in Case Reports in Pulmonology.
Recognizing Streptococcus intermedius (S. intermedius), which lives in the oral cavity, as an aggressive pathogen in pyopneumothorax may be important for early diagnosis and treatment, the authors wrote.
“This case is unique because pyopneumothorax secondary to S. intermedius is exceedingly rare, and prior reports more often involve individuals with risk factors such as dental disease, diabetes, or alcohol use,” wrote the authors, led by Dr. Justin Thomas of the Eisenhower Medical Center in Rancho Mirage, CA.
A healthy woman with shortness of breath and cough
A 52-year-old woman with no remarkable medical history went to a hospital emergency room with shortness of breath and a monthlong productive cough. The woman had no history of smoking or drinking alcohol. She had swelling in her legs and had lost about 20 pounds over a three-month period but had no other signs of infection. Previously, she had been given antibiotics and steroids, but her symptoms had not improved.
At the hospital, she had a 102° fever, and she was wheezing. A chest x-ray showed a hydropneumothorax, and a computed tomography (CT) chest scan with contrast “revealed a small burden of left-sided acute pulmonary embolism (PE), a large thick-walled irregular cavitary consolidation or mass in the right upper lobe (RUL) with an internal air-fluid level, and a moderate right-sided loculated hydropneumothorax/empyema.” Furthermore, she underwent an ultrasound that showed “bilateral nonocclusive, acute appearing deep venous thrombi (DVT) in the right popliteal, left superficial femoral, and left popliteal veins,” according to the case report.
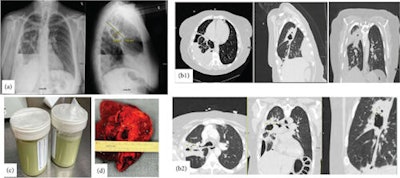 Figure 1: (a) Initial chest x-ray upon presentation showing extensive heterogeneous right lung opacity, which appears to be a thick-walled cavitary lesion about 4.8 × 10.5 cm. Moderate right loculated hydropneumothorax at the lung base with associated air-fluid level, concerning for empyema. (b) b1: A thick-walled cavitary consolidation or lesion in the posterior right upper lobe. There is a complex moderate right pleural effusion with air-fluid levels, concerning for empyema. There is extensive parabronchial thickening in the right lung. b2: CT chest after chest tube insertion; the yellow marker is pointing to a bronchopulmonary fistula, which was the reason for her continuous air leakage. (c) Frank pus after inserting the chest tube. (d) Right upper lobe abscess after lobectomy.Image and caption courtesy of Zohouri et al. Licensed under CC BY 4.0.
Figure 1: (a) Initial chest x-ray upon presentation showing extensive heterogeneous right lung opacity, which appears to be a thick-walled cavitary lesion about 4.8 × 10.5 cm. Moderate right loculated hydropneumothorax at the lung base with associated air-fluid level, concerning for empyema. (b) b1: A thick-walled cavitary consolidation or lesion in the posterior right upper lobe. There is a complex moderate right pleural effusion with air-fluid levels, concerning for empyema. There is extensive parabronchial thickening in the right lung. b2: CT chest after chest tube insertion; the yellow marker is pointing to a bronchopulmonary fistula, which was the reason for her continuous air leakage. (c) Frank pus after inserting the chest tube. (d) Right upper lobe abscess after lobectomy.Image and caption courtesy of Zohouri et al. Licensed under CC BY 4.0.
Due to the woman’s severe penicillin allergy, she was given broad-spectrum antibiotics intravenously, as well as heparin for the pulmonary embolism. On her second day at the hospital, a chest tube was inserted and pus was aspirated. Though analysis showed no malignant cells, it showed marked inflammation consistent with empyema. She received intrapleural fibrinolytics and underwent bronchoscopy with bronchoalveolar lavage and biopsy, the authors wrote.
Her antibiotics were changed due to a persistent fever, and her white blood cell count continued to rise. Culture results showed moderate growth of S. intermedius.
A maxillofacial CT showed no signs of sinusitis or abscesses. On her sixth day in the hospital, the woman underwent a right video-assisted thoracoscopy and thoracotomy, which revealed a large abscess in the right upper lobectomy.
Cultures from the abscess grew Corynebacterium tuberculostearicum, but these results were not finalized until the woman died. Due to its delayed growth and that it is a skin bacterium, it was not considered the pathogen that caused the woman’s condition, they wrote.
After successfully undergoing thoracic surgery, the woman developed unexplained cardiac arrest a few hours later and died.
What to know about this oral bacteria
The usually harmless S. intermedius can act as an opportunistic pathogen that causes severe infections, including brain and liver abscesses. However, S. intermedius’ involvement in pleuropulmonary infection (PPI), including parapneumonic effusion, is extremely rare.
In this case, the authors believe S. intermedius was the primary pathogen because it was isolated early from pleural fluid cultures. Also, the culture yielded a moderate growth of the oral germ in a sterile compartment. Those factors, combined with the presence of no other pathogens at the time of collection, uphold its clinical relevance, the authors wrote.
“This case highlights the pathogenic potential of S. intermedius, a typically benign oral commensal, to cause severe PPI even in previously healthy individuals,” Thomas and colleagues wrote.