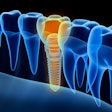
In patients with chronic periodontitis, implant design, implant length, and inflammation may be key risk factors for bone loss and implant fractures and failure. This study was recently published in BMC Oral Health.
Furthermore, these patients have a higher risk of developing mucositis and peri-implantitis after dental implant surgery, the authors wrote.
"Chronic periodontitis patients after dental implant surgery increase the risk of bone loss, the prevalence of mucositis and peri-implantitis," wrote the authors, led by Qiang Zhang of the Second People's Hospital of Changzhi in China (BMC Oral Health, September 8, 2024, Vol. 24, 1051).
The study comprised 284 patients with a mean age of about 45 who sought implants. Of the patients, 128 were periodontally healthy patients and 156 had chronic periodontitis.
Patients received implants with standard, standard-plus, or tapered designs, with diameters ranging from 4.1 mm to 4.8 mm and lengths of 8 mm, 10 mm, or 12 mm. The study assessed the impact of implant design on the crestal bone level (CBL) and marginal bone loss (MBL) as risk factors for implant failure, they wrote.
Clinical parameters such as probing depth (PD), sulcus bleeding index (SBI), plaque index (PLI), gingival bleeding (GIL), and bleeding on probing (BOP) were measured to evaluate peri-implant conditions. The prevalence of mucositis and peri-implantitis was determined using a manual periodontal probe. Venous blood samples were collected at baseline and three, six, nine, and 12 months. Serum was extracted via centrifugation, and levels of inflammatory cytokines, they wrote.
At six months after implant placement, CBL differences, which were influenced by implant diameter, between the groups became significant. In patients with periodontitis, larger implant diameters and lengths were associated with increased MBL. Tapered implant designs resulted in lower MBL compared to standard and standard-plus designs in chronic periodontitis patients, according to the study.
Periodontally healthy patients had lower PD and SBI. Chronic periodontitis patients also had higher PLI, GIL, and BOP. Chronic periodontitis patients showed elevated serum levels of tumor necrosis factor alpha, interleukin 6, interleukin 1, matrix metallopeptidase 2, and matrix metallopeptidase 9 postsurgery.
Additionally, chronic periodontitis patients had a higher prevalence of mucositis (14.5% versus 4.7%) and peri-implantitis (20.2% versus 6.0%) compared to healthy patients.
Most failures in chronic periodontitis patients were linked to peri-implantitis and biomechanical load, with tapered designs having higher survival rates. The incidence of implant fractures was higher in chronic periodontitis patients (7.3% versus 3.3%). Long implant lengths and diameters increased fracture rates in periodontitis patients, while tapered designs reduced fracture incidence. Overall, implant failure rates were 14.3% for periodontitis patients and 4.9% for healthy patients, according to the results.
The study, however, had limitations. It did not examine the effects of patient age, chronic periodontitis treatment outcomes, or the severity of the condition on dental implant failure, the authors wrote.
"The data of this study highlight risks to consider when trying to prevent bone loss and further failure of dental implant reported cases of chronic periodontitis patients," Zhang and colleagues wrote.