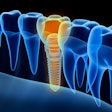
Short implants may provide a simpler alternative to more invasive surgical techniques, making them a viable option for prosthetic rehabilitation in edentulous patients. This study was recently published in the Journal of Prosthetic Dentistry.
Though lower survival rates have been reported, the design of the implants and the operator's expertise play roles in their success, the authors wrote.
"Short implants are a therapeutic solution to more complex surgical techniques," wrote the authors, led by Dr. Carlos M. Cobo-Vázquez, PhD, MSc, of the Complutense University of Madrid in Spain (J Prosthet Dent, September 12, 2024).
The randomized clinical study involved volunteers enrolled between September 2018 and September 2020 through the Master of Oral Surgery and Implantology and the implant prosthodontics program at San Carlos Clinical Hospital in Spain. A total of 14 participants (six men and eight women) with an average age of approximately 63 received 61 implants: 36 with external connections and 25 with internal connections.
Implant type, type of opposing tooth, and the presence of at least 2 mm of keratinized gingiva were recorded on the day of implant placement and at three, six, 12, and 24 months. A simplified hemorrhage index and a simplified calculus index were evaluated. A descriptive analysis was performed along with a binary logistic regression model using generalized estimating equations, and implant survival was analyzed, they wrote.
At the 24-month follow-up, the estimated survival rate was 85.2% (95% confidence interval [CI]: 76.8%-94.6%). By the final follow-up, survival was 80% (95% CI: 65.8%-97.3%) for the internal connection group and 88.9% (95% CI: 79.2%-99.8%) for the external connection group, with no significant difference between them (p = .308). A band of keratinized mucosa of at least 2 mm was present in 35% of internal connection implants compared to 63.6% of external connection implants, according to the results.
Bone loss increased over time, but no significant differences were observed between connection types (p = .311). Bleeding on probing was observed in 28 implants, with a higher prevalence in external connection implants (57.6%, p = .025). Plaque was present in 36 implants, though no statistically significant differences were found between external (72.8%) and internal connections (60.0%, p > .05).
A total of 28 implants had at least 2 mm of keratinized mucosa, but the difference between external (63.6%) and internal connections (35.0%) was not statistically significant (p = .200). Eight complications (13.1%) were reported, including connection fractures, a screw fracture, a framework fracture, and buccal fenestrations, according to the results.
The study had limitations, including a small sample size, which limited the statistical analysis and the significance of the results, the authors added.
"Difficulties were encountered in achieving primary stability in surgery due to the implant length and the need for precise milling," they wrote.