In the beginning, it was not believed that the periodontal ligament cells were responsible for the healing of the periodontium. It was widely believed at one time that the cells responsible for regenerating the periodontium were derived from the alveolar bone.
It was not until the late ’80s and early ’90s that conclusive evidence was found in experiments with monkeys that the progenitor cells in the periodontium were responsible for the regeneration of the periodontal apparatus.
It was hypothesized that greater regenerative capability could be achieved by isolating the progenitor cells of the periodontal ligament (PDL) and alveolar bone, allowing them to repopulate without interference from the faster-growing epithelium and gingival connective tissue. This led to the development of membranelike barrier materials and the emergence of the concept known as guided tissue regeneration (GTR).
 Dr. John Zalesky.
Dr. John Zalesky.
To selectively guide periodontal regeneration following disease, flap surgery was performed on monkeys that had been exposed to plaque for six months. A cellulose acetate laboratory filter or expanded polytetrafluoroethylene (ePTFE) membrane was used to prevent gingival connective tissue from contacting the root surface during healing, thereby maintaining space for PDL tissue ingrowth. After three months of healing, histologic evaluation showed that test sites protected by the membrane exhibited significantly more new attachment and bone growth due to the prevention of epithelial downgrowth.
Subsequently, the general principles of guided bone regeneration (GBR) were introduced by providing the cells from bone tissues to regenerate uninhibited by the epithelial through the utilization of a barrier membrane, and the concept took hold and changed the way we regenerate oral bone and the PDL today.
Since 2019, BioHorizons and Camlog have been committed to the development of evidence-based and scientifically tested products on the dental market. Through this collaborative effort, they have become a global provider of regenerative solutions for implant dentistry and cover the needs of a large portion of clinicians looking to improve the outcomes of their surgical procedures.
In early 2024, they launched a new product, Striate+, an innovative porcine-derived collagen membrane developed by Orthocell for advanced bone and tissue regeneration. Striate+ is the next generation of collagen membranes. The manufacturing process, referred to as Scaffold Matrix Regenerative Therapy, removes all traces of DNA and immunogenic contaminants, resulting in a highly purified, biocompatible membrane while preserving the structure of the native collagen.
Striate+ has several optimal indications, which include immediate extraction sites, delayed extraction sites, GBR, GTR, and various periodontal defect regeneration. The rapid and predictable bone regeneration observed after guided bone regeneration with Striate+ improves long-term survival and aesthetic outcomes.
Striate+ is a non-cross-linked, acellular type I collagen, which does not induce an abnormal inflammatory response and minimizes the risk of wound dehiscence. Its innovative bilayer design allows it to readily conform to bone surfaces.
The smooth and rough sides allow it to stimulate specific biological responses. The smooth side facing the soft tissue consists of densely packed collagen bundles arranged in parallel, which, in their barrier function, prevent the migration of the epithelial cells into the defect.
The rough side, which faces the bone defect, consists of a porous network of collagen fibers, forming an open scaffold promoting osteogenesis, referred to as the "bioactive chamber". Thus, Striate+ was developed to protect the bone graft from epithelial cell ingrowth and to create a favorable environment for osteogenesis, with a predictable resorption time for protected bone regeneration.
Furthermore, Striate+ exhibits excellent handling and usability. It can be applied without prior hydration, gently adheres and conforms to a defect, and can be stabilized by suturing. I found Striate+ to have a higher mechanical strength than other products on the market. The membrane absorbs fluids by capillarity but does not swell excessively, facilitating primary closure and making it particularly suitable for patients with a thin periodontal biotype.
Seven practitioners, including both general dentists and periodontists who serve as clinical product evaluators for Catapult Education, were given the Striate+ collagen membrane to use in their everyday clinical cases.
 Dr. Gordon Fraser.
Dr. Gordon Fraser.
These advanced procedures included but were not limited to implant placement, bone regeneration, and tissue repair. As evaluators, we focused on its handling, adaptability, effectiveness, and versatility for achieving predictable clinical outcomes in various surgical scenarios. At the end of the evaluation period, we were all asked to provide unbiased feedback based on our clinical experience with Striate+.
We found Striate+ to be highly adaptable to various surgical scenarios. In comparison with other commonly used brands on the market, we noted positive feedback for its enhanced handling and adaptability. A significant majority rated Striate+ as “better” or “much better” than their current membranes, emphasizing its advantages in challenging surgical situations.
The typical challenges with other membranes, which were minimized with Striate+, include loss of control at placement, difficult manipulation, decreased rigidity/stiffness when moistened, and collapse into the site. Striate+ was particularly well received for its handling, with around half of evaluators rating it as “better” and a third as “much better” compared to their customarily used membranes. Evaluators favorably noted its ability to “conform well to the site” without excessive rigidity, making placement easier.
Postoperative outcome feedback was also positive, with evaluators observing effective wound support and healthy tissue response with minimal inflammation and smooth integration. Comments such as “The site looked surprisingly nice,” and “The tissue was healthy, no inflammation,” highlight its biocompatibility and suitability in various surgical procedures.
Overall, Striate+ was well received by Catapult’s evaluators. Its advanced collagen membrane design supports effective handling, adaptability, and favorable healing outcomes, making it a reliable choice for surgical procedures requiring high-quality membrane support.
Catapult Education has established several key criteria to determine whether a product receives the Catapult Vote of Confidence™. Based on our clinical experience with Striate+ and the results we achieved, all participating practitioners agreed that Striate+ is a product we would confidently incorporate into our own practices to support optimal surgical outcomes -- and one we would readily recommend to our colleagues.

It is our pleasure to award Striate+ the Catapult Vote of Confidence, as it continues to prove itself as a valuable tool for bone and soft tissue regeneration.
Clinical application
An 18-year-old high school senior presented with a history of tooth avulsion at #9. The injury occurred while she was roughhousing with her younger brother, whose head struck her mouth, fracturing the tooth at the cementoenamel junction. Tooth #10 also showed an incisal edge fracture. The patient reported no pain, as she had taken ibuprofen prior to the visit.
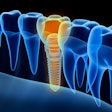
Radiographs and a cone-beam computed tomography scan were obtained, and it was determined that the appropriate treatment plan would be to extract the remaining root of #9 and place an immediate implant. When placing an immediate implant into an extraction site, it is critical to graft the space around the implant to preserve bone volume.
In this case, our primary concern was maintaining the buccal bone and creating an ideal emergence profile while ensuring symmetry with tooth #8. In addition to the bone graft, a resorbable membrane was placed to support these objectives. The implant at #9 was then placed and allowed to heal for four months.
During the healing phase, the patient wore a flipper to replace #9. When the implant was ready for restoration, the tissue punch technique was used to place the healing abutment. This abutment helped shape the gingiva in a cufflike manner, allowing the final restoration to emerge naturally from the tissue.
As seen in the final result, we successfully achieved our objectives, and our patient is now off to begin her freshman year of college with a confident smile.
 Figure 2-11: Initial uncovering of the implant reveals the need for additional augmentation to achieve an adequate soft tissue profile. A palatal releasing incision was made to avoid scarring in the aesthetic zone, followed by full-thickness reflection to the facial bone in preparation for hard and soft tissue augmentation.All images courtesy of Dr. Gordon Fraser.
Figure 2-11: Initial uncovering of the implant reveals the need for additional augmentation to achieve an adequate soft tissue profile. A palatal releasing incision was made to avoid scarring in the aesthetic zone, followed by full-thickness reflection to the facial bone in preparation for hard and soft tissue augmentation.All images courtesy of Dr. Gordon Fraser.
 Figure 3-11: Residual defect -- or "moat" -- around the implant observed upon full-thickness reflection. The void was filled with cortical/cancellous bone graft material.
Figure 3-11: Residual defect -- or "moat" -- around the implant observed upon full-thickness reflection. The void was filled with cortical/cancellous bone graft material.
 Figure 4-11: Placement of the Striate Membrane (BioHorizons) to prevent soft tissue ingrowth during the regenerative process.
Figure 4-11: Placement of the Striate Membrane (BioHorizons) to prevent soft tissue ingrowth during the regenerative process.
 Figure 5-11: Facial tissue is approximated to assess the parameters needed for achieving primary soft tissue closure.
Figure 5-11: Facial tissue is approximated to assess the parameters needed for achieving primary soft tissue closure.
 Figure 6-11: Palatal view of tissue approximation to achieve primary soft tissue closure.
Figure 6-11: Palatal view of tissue approximation to achieve primary soft tissue closure.
 Figure 7-11: Striate+ Membrane placed over grafted bone and implant, ensuring intimate contact with the membrane.
Figure 7-11: Striate+ Membrane placed over grafted bone and implant, ensuring intimate contact with the membrane.
 Figure 8-11: Unlike most membranes on the market, the Striate Membrane is easily cut and placed. Here, we check for proper site fill before closure.
Figure 8-11: Unlike most membranes on the market, the Striate Membrane is easily cut and placed. Here, we check for proper site fill before closure.
 Figure 9-11: Final primary closure of the site.
Figure 9-11: Final primary closure of the site.
 Figure 10-11: Tooth #9 with healing cap.
Figure 10-11: Tooth #9 with healing cap.
 Figure 11a-11: Final restoration of tooth #9.
Figure 11a-11: Final restoration of tooth #9.
 Figure 11b-11: Final restoration of tooth #9.
Figure 11b-11: Final restoration of tooth #9.
Editor's Note: Learn more from Dr. Zalesky in the video below.
The comments and observations expressed herein do not necessarily reflect the opinions of DrBicuspid.com, nor should they be construed as an endorsement or admonishment of any particular idea, vendor, or organization.
Dr. John Zalesky received his Master of Biomedical Science from the University of Medicine and Dentistry at the New Jersey School of Biomedical Sciences. He was awarded his Doctor of Medicine in Dentistry degree from the Nova Southeastern University College of Dental Medicine, and he completed a general practice residency at Denver Health Medical Center. He is a fellow of the Academy of General Dentistry and the International Congress of Oral Implantologists. Dr. Zalesky has been published in several respected dental journals.
Dr. Gordon Fraser is a graduate of Temple University and served our country as a periodontist in the U.S. Air Force. Dr. Fraser is the founder of Pure Perio, a dental implant coaching program. He is the founder of the Southern Georgia Dental Education and is a member of the American Academy of Periodontology, the ADA, the Georgia Dental Society, the National Dental Association, the North Georgia Dental Society, and the Catapult Education Speakers Bureau.