The use of a continuous positive airway pressure (CPAP) mask and machine may have led a man’s dental prosthesis to fail, highlighting this sleep apnea therapy as a possible high-risk factor for implant failure. The case report was published on May 18 in the Journal of Prosthodontics.
Until the immediate failure of the 71-year-old man’s full-arch implant prosthesis, there have been no reported cases of CPAP machine usage as a risk factor for implant failure. After the failure, the man refrained from using the CPAP machine for three weeks as instructed by his dentist and sleep doctor, and a revision implant surgery was successfully completed, the authors wrote.
“It is imperative that the dental profession is aware of the risks of CPAP machine use during early osseointegration periods of full-arch implant-supported restorative treatment,” wrote the authors, led by Dr. Neeraj Surathu of Nova Southeastern University in Fort Lauderdale, FL.
A 71-year-old man wanting a new smile
The patient went to the dentist looking to have his lower teeth restored. Imaging and a clinical exam showed terminal lower jaw dentition due to compromised stage II, grade B periodontal status and mobility.
The man reported no allergies, was a former smoker, and took medication to control high cholesterol, as well as aspirin and multivitamins. It wasn’t until after the initial all-on-four dental implant surgery and immediate loading was completed that the patient revealed his diagnosis of sleep apnea and that he used a CPAP at night for treatment, the authors wrote.
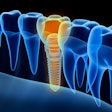
The patient underwent a full-arch extraction of his mandibular teeth, an immediate implant placement, and an immediate insertion and load of a mandibular fixed prosthesis. Periodontal treatment and fixed partial dentures in the maxilla would be done after the first procedure. The man underwent the agreed-upon restorative treatment without any complications on the day of surgery, they wrote.
Twenty-four hours after the postoperative visit, the patient was called, and he reported little swelling and no pain. At his next appointment, 10 days after the procedure, the man reported increasing discomfort and minor swelling.
An exam revealed wide open flaps with extensive bone exposed in the anterior area of the mandible. The bone was cleaned, and a layer of necrotic bone was carefully removed. Also, bone was removed at the flaps’ margins to improve the primary closure. The implants and prosthesis, however, remained stable. The man was told to return in four weeks for reevaluation and removal of the sutures.
Four weeks later, when the man returned, the flaps looked reopened and were exposing a considerable amount of bone. The clinician removed the conversion prosthesis to access the implants and surrounding bone.
The prosthesis was mobile and easily removed, including the implants, when the seals were removed from the screw access channels. As the prosthesis was removed, significant facial and lingual cortical plates remained attached to the implants.
The clinician then removed the tissue and necrotic bone. The remaining bone was scrapped to cause bleeding, which indicated vital bone with the possibility of new bone formation. The site was irrigated, and the primary closure was sealed with one suture.
At this time, the patient reported his nightly use of a CPAP machine. The dentist told him to stop using the machine for three weeks, and the patient’s sleep doctor agreed and instructed him to control his chronic sleep apnea by sleeping with his head elevated, according to the report.
After three weeks, the patient returned for suture removal and reevaluation of the existing bone. His soft tissue had healed, and he underwent a cone-beam computed tomography scan to plan for new implants.
Based on his available bone and the remaining bone, the patient agreed to revision surgery with NobelSpeedy Groovy external hex design implants. Astra EV Osseospeed implants were used for the first procedure.
The patient underwent a lower jaw complete denture implant-supported hybrid prosthesis, which is eight times stronger than a traditional lab-processed polymethyl methacrylate prosthetic, on five implants. Three implants were placed in the intermorainal region and two were placed posterior to the mental foramen. To avoid cantilever with early implant loading, the two posterior implants were placed bilaterally. The procedure was completed over several weeks, the authors wrote.
At the patient's postoperative visit, he was pleased with the look and feel of his restorations. He was placed on a four-month recare plan, according to the report.
A contributing factor for implant failure
Currently, nonsmokers and patients with no history of diabetes, bisphosphonate use, those with systemic blood pressure within normal limits, and no parafunctional habits are good candidates for implant reconstruction. However, this case suggests CPAP use may be a “high-risk” factor that contributes to implant failure due to the mechanical pressure the machine’s mask puts on the mucosal flap closure, positive air pressure on the bone, and bacteria that are pushed under the mucosal flaps from the sleep apnea machine’s tube, the authors wrote.
Since catastrophic dental implant failure is a major physical, psychological, and financial loss to a patient, if CPAP use is revealed during screening, the person may need to take a hiatus from using it before and after surgery. Taking this step likely will prevent any primary implant failure related to the adverse effects of wearing a CPAP mask, according to the report.
With the rise of implant-supported surgical treatments and the protocol of giving patients teeth in a day, it’s important that dentists are informed about the risk factors of using a CPAP machine when dental implants are placed. More research should be conducted to better understand the short-term side effects of CPAP usage and complications with osseointegration, the authors wrote.
“This patient treatment has demonstrated that sleep apnea and subsequent CPAP machine usage as a new landmarked risk factor demonstrated in this patient contribut[ed] to primary implant failure,” Surathu and colleagues wrote.