ANAHEIM, Calif. - Infected tooth? Replace it! With the rapid improvement in implantology, that kind of thinking comes easily, but in many cases, endodontics still offers a better alternative, Jerome H. Stroumza, D.D.S., M.S., D.Sc., told an audience Thursday at the California Dental Association (CDA) Spring Scientific Session.
"The trend now is probably to extract too easily and forget what endodontics can do," said Dr. Stroumza, who has combined the two specialties at his EndoImplantology Institute in San Francisco.
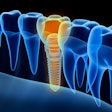
Implants have progressed dramatically in recent years, particularly with the improvement in bone grafting materials and growth factors, Dr. Stroumza said. And in many cases, he places implants where they would not have been possible a decade ago.
But using endodontics, he also saves many teeth that have already been unsuccessfully restored by another dentist.
So how do you know when to give up? The key is to carefully analyze the long-term prognosis, the patient's expectations, and the risk versus the benefit, Dr. Stroumza said.
In some cases, patients are deeply attached to their teeth and will be grateful -- and willing to pay -- for heroic efforts to save them. "In the worst case, you fail, then you go on to the other approach," he said.
In other cases, implants are not likely to succeed because the bone condition is so poor that even bone grafting techniques can't help.
One way to figure out which teeth can be saved is through the use of CT scans, Dr. Stroumza said. He showed examples of cases in which CAD/CAM images produced by a CT scan showed that a canal could not be found, and other cases in which there was insufficient bone to support an implant.
"I used to do a lot of exploratory surgery, but now we have the CT scan -- it's almost like you're right there," he said.
The use of CT scans for endodontology was the biggest revelation in Dr. Stroumza's talk, said Arthur Schultz, D.D.S., a general dentist in Manhattan Beach, Calif. "I had never heard of that before," he said.
But CT scans are not the only technique Dr. Stroumza uses to decide whether to do a root canal or place an implant. In another case, a cast helped him model the occlusion of two posterior molars and decide that both had to be replaced with implants.
What other factors should a clinician consider? The type of lesion shouldn't determine the type of therapy you use, and neither should the mobility of the tooth, Dr. Stroumza said. He gave the example of a tooth so mobile that he "didn't want to put a dam around it because the dam might extract it." After the root canal, however, the bone regenerated enough to support the tooth.
It was one of many cases in which he has found that eliminating endodontic infection encouraged bone growth. "Osteoplastic cells will not migrate if you have toxicity, but if you really remove what's wrong, the bone will grow," he said.
That's why he emphasizes proper cleaning, shaping, and disinfection. "I don't know why people rush to pack," he said. "Packing has no value; cleaning and shaping has the value."
As for sealing the tooth, Dr. Stroumza prefers amalgam to composite resins. "My confidence in plastic is very limited," he said. On the other hand, if he even suspects there is a crack, he uses composite resins because even a little pounding can do damage.
But in addition to making use of such classic endodontic techniques, Dr. Stroumza also wields the latest tools in implantology, and he talked as well about the use of platelets in implant sites.
Ultimately, he said, the two approaches are not in opposition. "In truth, there is no battle between endodontics and implantology," he said. "You can get the best of both."