Dental x-rays revealed that a healthy 28-year-old man developed apical periodontitis in two teeth following an intense phase of bruxism that lasted about a year, according to a case report published March 24 in BMC Oral Health.
This is believed to be the first clinical case of apical periodontitis caused solely by bruxism, the authors wrote. Additionally, this case highlights the importance of taking complete medical histories and routine x-rays of patients, they wrote.
"Practitioners need to be informed that intense bruxism can possibly lead to apical periodontitis," wrote the authors, led by Dr. Madline Gund, of the Clinic of Operative Dentistry, Periodontology and Preventive Dentistry, Saarland University Hospital at Saarland University in Homburg, Germany.
28-year-old man with increasing apical osteolysis
A healthy 28-year-old man with apical periodontitis on tooth #36 and #46 was referred by his primary dentist to the dental clinic at Saarland University. Though endodontic treatment had already begun, apical osteolysis was increasing on both teeth, according to the case report.
The patient's primary dentist could not determine the cause of the apical periodontitis. The teeth had no fillings or caries, nor had the patient experienced trauma or an accident. Further, he did not have any periodontal problems, the authors wrote.
Upon examining the teeth, the dentist observed increased tooth mobility and bifurcation at a probing depth of 4 mm. The periodontal screening index was unremarkable, showing no signs of periodontal disease. However, tooth #36 and #46 each showed a 10-mm pocket with bleeding on probing at the vestibular central, and there was some bulging elastic swelling at the vestibulum, they wrote.
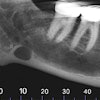
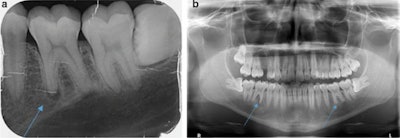
 The patient's routine x-ray taken by a primary dentist in January 2019 reveals that tooth #36 and #46 showed no signs of apical osteolysis before the intense bruxism started. The teeth also did not show visible signs of caries or fillings. All images courtesy of Gund et al. Licensed by CC BY 4.0.
The patient's routine x-ray taken by a primary dentist in January 2019 reveals that tooth #36 and #46 showed no signs of apical osteolysis before the intense bruxism started. The teeth also did not show visible signs of caries or fillings. All images courtesy of Gund et al. Licensed by CC BY 4.0.A percussion test was negative, and the exam and imaging revealed no anomalies, pulp calcifications, or formation defects of the hard tooth tissue. Also, there was no external resorption, root canal, or pulp chamber perforation, according to the report.
While taking his medical history, the man reported that he first felt pain on the right side of tooth #46 about a year and a half before the visit. It was a radiating, pulling, and difficult-to-localize pain. The pain pulsated before he went to bed.
With the pain, the man experienced an earache and temporomandibular joint pain. He experienced percussion pain for two days before it disappeared. His primary dentist did a percussion test that was negative and a sensibility test that was reduced, the authors wrote.
Since the patient's primary dentist was unable to identify an odontogenic cause for his problems, the man was referred to an otolaryngologist. The otolaryngologist prescribed the patient a weeks' worth of antibiotics without a diagnosis. The medication completely resolved his pain.
Identifying the cause of the pain
About a month and a half later, the patient once again experienced the same pain again with tooth #46 and tooth #36. The patient underwent two x-rays ordered by an emergency dentist. This new dentist could not establish a diagnosis, so the patient was prescribed antibiotics but did not undergo treatment. The antibiotics resolved the pain once again, according to the report.
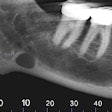
 a: An x-ray taken in October 2019 shows apical osteolysis in tooth #36. b: An x-ray taken in October 2019 shows apical osteolysis in tooth #36 and #46. The osteolysis is greater in tooth #46.
a: An x-ray taken in October 2019 shows apical osteolysis in tooth #36. b: An x-ray taken in October 2019 shows apical osteolysis in tooth #36 and #46. The osteolysis is greater in tooth #46.Then, two and a half months later, the patient's pain returned, prompting his primary dentist to take a new x-ray. This dentist diagnosed him with apical periodontitis on tooth #36 and #46, and he began endodontic treatment even though the teeth already appeared dead, the authors wrote.
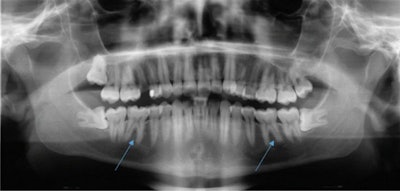
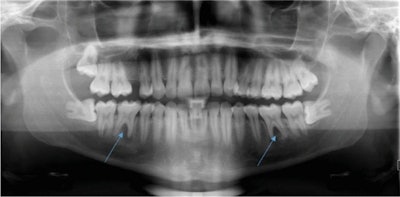 An x-ray taken in January 2020 shows apical and interradicular osteolysis on tooth #36 and #46.
An x-ray taken in January 2020 shows apical and interradicular osteolysis on tooth #36 and #46.When the attending dentist of the university hospital explicitly asked the patient what his life was like during the periods of pain, the patient confirmed experiencing a lot of stress due to the completion of his studies, as well as pressing his teeth at night, according to the report.
About one and a half years after his initial pain began -- and about two weeks before endodontic treatment started -- the patient wore a bite splint. Around the same time, clinicians at the university prepared his teeth for root canals to treat the apical periodontitis.
During a follow-up visit two weeks later, the patient reported having no pain. Also, the 10-mm pockets on the two teeth showed no bleeding on probing, and there was no mobility on tooth #46 and minimal mobility on tooth #36.
The clinicians went ahead and completed the root canals on the patient, the authors wrote. Since treatment has been completed, the patient has remained asymptomatic and regularly uses a bite split. One year after the root filling, he will undergo another x-ray.
Common condition, multiple outcomes
As many as 1 in 5 people will experience bruxism, which can lead to several conditions, including tooth fractures, muscle pain, occlusal trauma, and even damaged pulp. Numerous factors, including stress, genetics, alcohol or caffeine consumption, and illegal drug use, may be involved in the origin of bruxism.
Though experimental consequences of occlusal trauma to the pulp have been described in previous literature, authors believe this case of apical periodontitis is the first strictly due to bruxism.
In cases involving unexplained tooth pain, possible bruxism should be clarified when medical histories are taken, because they may indicate apical periodontitis in the context of dental trauma. Furthermore, more studies are needed to conclusively address the connection between bruxism and apical periodontitis, Gund and colleagues concluded.
"[In this case], the etiopathogenesis of the apical periodontitis was explained by a diagnosis of exclusion, since neither tooth had caries, fillings, or undergone trauma," the authors wrote.