Cone-beam computed tomography (CBCT) clearly maps the neurovascular canals and the anatomic variants of patients' upper and lower jaws, facilitating the safe performance of endodontic treatments, according to a case series published on September 15 in the Journal of Endodontics.
CBCT imaging provides accurate, high-resolution visualization of the accessory canals of the jaws along with tools to evaluate areas of interest in detail and map the communications of accessory neurovascular channels with the main neurovascular bundle. This allows endodontists to provide better diagnoses and treatment planning, the authors wrote.
"Comprehensive evaluation of the CBCT scans demonstrated relevant underlying etiopathologies, prompting clinical modifications that led to enhanced patient outcomes," wrote the group, led by Dr. Vandana Kumar from the department of oncology and diagnostic sciences at the University of Maryland School of Dentistry.
Endodontists often treat patients with complex conditions, such as apical periodontitis, root resorption and perforation, atypical root canal forms, traumatic dental injuries, and obturation problems. Imaging is crucial to managing the diagnosis and treatment planning of these conditions. 3D imaging, such as CBCT, avoids most of the intrinsic limits that occur with 2D imaging, such as superimposition of overlying anatomy and distortion. Additionally, 3D images of the maxillofacial anatomy can be reformatted in different planes, enabling visualization of anatomically abnormal cases.
CBCT imaging can be used to identify the causes of associated diseases in patients with endodontic problems, which is showcased in four unique cases in this series.
A 26-year-old man
A man with no significant medical history visited an endodontist because he was experiencing extraoral swelling in the mandibular anterior region. In 2014, he experienced trauma to that area and his mandibular left lateral incisor underwent a root canal in 2016 and again in 2018.
An exam showed that the mandibular left canine was discolored and tested nonvital. An x-ray revealed a low-density lesion at the apical regions of the mandibular left lateral incisor and canine and a small well-defined low-density lesion within the apical third of the mesial aspect of the root of the lower left canine. Internal root resorption was suspected, according to the authors.
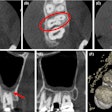
A CBCT scan was performed and showed a localized distal periodontal defect suggestive of oblique root fracture in the man's lower left second premolar. The scan revealed a tubular-shaped vascular channel in the apical third of the root of the lower left canine. It extended mesiodistally with a lingually inclined orientation and reached the pulp canal. This allowed inflammatory cells and fluid to seep along the distal and mesial root surfaces, which contributed to two periapical low densities.
The smaller zone was along the distal root surface, and the larger zone shared with the adjacent lateral incisor that measured approximately 14 mm. The diagnosis of internal resorption defect was ruled out because the mapped tubular accessory vascular channel revealed a developmental vascular defect. CBCT helped make the most appropriate treatment plan for the patient.
During treatment, the endodontist aspirated a bloody, purulent fluid when the man's pulpal chamber was accessed. Calcium hydroxide was applied into the root canal system and the tooth was sealed six weeks later.
An 80-year-old man
A man experienced persistent pain arising from the mandibular right posterior region, so he visited an endodontist. A sinus tract associated with a deep amalgam restoration on the mandibular right second molar was discovered during an exam. An x-ray revealed a periapical low-density region at the apical region of the mandibular right first molar and distal crestal bone loss.
A CBCT scan revealed periapical low-density regions of the mesial and distal roots of the mandibular right first molar. It also identified a distal root of the lower right second molar, extending to the inferior aspect of the clinical crown of the horizontally impacted mandibular right third molar. The first molar displayed bone loss at the branching point of the tooth root, as well as resorption of the buccal cortical plate. The lesions appeared to be continuous with mapped prominent accessory vascular channels that communicated with the right lower canal. The accessory vascular channel was identified just below the apical region and on the buccal aspect of the mandibular right second premolar. This finding was comparable to the lesion seen on the x-ray, signifying that the radiographic finding didn't have an endodontic origin, according to the authors.
The CBCT also alerted the endodontist to the patient's increased risk for excessive bleeding during apical surgery or extraction. The man's lower right first, second, and third molars were extracted successfully, and no other treatment was performed, the authors wrote.
A 23-year-old woman
A woman went to the University of Maryland School of Dentistry for endodontic treatment of her lower left second molar and to have a partially erupted lower left third molar pulled. An x-ray showed that her lower left second molar had a periapical low-density region associated with extensive mesial caries invading the pulp chamber. It also showed a mesially inclined mandibular left third molar.
A CBCT scan showed an abnormal division of the left mandibular canal. It branched superiorly from the distal of the mandibular left second molar and coursed mesially to run buccal to the apical region of the distal root of the mandibular left second molar. In addition, a second vascular channel was located more superiorly along the distal surface of the mandibular left first molar. From there, a second canal moved distally, and this canal passed through the mesial root of the mandibular left second molar, the authors wrote.
The mesiolingual apex of the mandibular left second molar appeared shortened due to the anomalous canal. The CBCT allowed the clinician to timely revise the woman's treatment plan and prevented the patient from having a traumatic extraction. She successfully underwent endodontic therapy on the lower second molar, they wrote.
A 40-year-old woman
A woman who had a sensitive and slightly mobile maxillary left central incisor went to an endodontist. The tooth had undergone a root canal for irreversible pulpitis four months earlier. A CBCT scan showed periapical low densities associated with the endodontically treated maxillary left central incisor. A closer look showed multiple vertically oriented, corticated, curvilinear low densities near both maxillary central incisors. This was consistent with accessory neurovascular channels and was characterized as an anatomical variation of the canalis sinuosus. A similar curved line accessory neurovascular channel was seen in the apex region of the maxillary right first premolar, the authors noted.
Based on the CBCT, the damaging masticatory forces were eliminated to stabilize the tooth. The patient chose to defer any additional treatment. Her pain was gone within three weeks, they wrote.
Better views, better outcomes
These cases show that 3D imaging can offer relevant information about the causes of some unusual endodontic diseases, as well as modification of clinical management.
"It is advised that the detection of accessory canals on CBCT scans should prompt neurovascular mapping, particularly coincident with the presence of an endodontic pathosis or when performing presurgical planning for apical surgery, implant placement, bone grafting, or other surgical procedures," they concluded.