Is cone-beam CT (CBCT) ready to be used in implant dentistry? In a new review, researchers examined published studies on CBCT and provided up-to-date recommendations for its use.
The group searched relevant medical literature and found a wide range in radiation dose and image quality among the CBCT scanners studied. The use of CBCT is well-established in the preoperative stages of implant dentistry, the researchers reported, but they recommended restrictions on its current postoperative usage (BMC Oral Health, May 15, 2018).
“Dental CBCT could be justified for presurgical diagnosis, preoperative planning, and preoperative transfer for oral implant rehabilitation.”
"Dental CBCT could be justified for presurgical diagnosis, preoperative planning, and preoperative transfer for oral implant rehabilitation, whilst striving for optimization of CBCT-based machine-dependent, patient-specific, and indication-oriented variables," they wrote.
The lead author of the review was Reinhilde Jacobs, PhD, DDS, a professor in the University of Leuven Faculty of Medicine in Belgium and head of the Division of Oral and Maxillofacial Surgery - Imaging and Pathology.
Going 3D
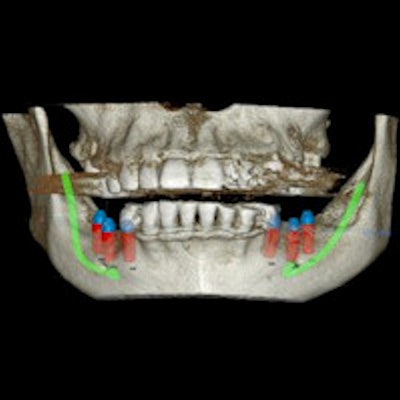
The success of CBCT in dentistry is due in part to its ability to perform volumetric jaw bone imaging at reasonable prices and relatively low doses using fairly compact equipment, the authors noted. Additionally, in implant dentistry, the 3D data are useful not only for diagnostics but also for surgical implant planning.
However, with significant technological advances in imaging, digital technology, and CAD/CAM systems -- and more than 85 CBCT devices available -- simplified solutions are needed, they wrote.
Jacobs and colleagues searched for studies published in English through November 2016. They noted that there is a gap between the existing literature and the available hardware and software.
"Research findings cannot simply be generalized as published evidence may often refer to one CBCT machine and not necessarily apply to other equipment," they wrote.
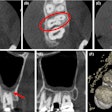
Based on the literature, indications for presurgical use of CBCT include the following, according to the group:
- Identification of critical anatomic boundaries
- Aesthetic challenges in the anterior maxilla
- Insufficient bone volume, shape, and quality
- Prevention of neurovascular trauma
- Augmentation procedures
- Use of advanced techniques, such as grafting, distraction, and zygomatic implants
- Suspected trauma history of jaws and teeth
- Doubtful prognosis of neighboring teeth
- Integrated presurgical planning and the use of a virtual patient approach
Dental CBCT has significant potential for uses beyond radiodiagnostics, including in the creation of surgical guides and for prosthetic rehabilitation via CAD/CAM procedures, according to numerous studies.
The authors noted enormous variations in radiation dose and image quality between CBCT machines, as well as a close relationship between image quality and radiation dose.
Typically, an effective radiation dose for CBCT should be the equivalent of two to 10 panoramic radiographs, they wrote. Low-dose protocols have been recommended in some studies, although research is needed to define the required image quality balanced with radiation dose output.
Voxel sizes of reconstructed CBCT datasets ranging from 0.08 mm to 0.4 mm are usually considered to provide high spatial resolution, studies have shown. Segmentation accuracy varies, which can be relevant when performing integrated virtual planning, including jaw bone models, fabrication of radiographic and surgical guides, and prosthetic models.
Other CBCT limitations include the lack of diagnostically distinct soft-tissue contrast, a lack of standardized grey value distribution that complicates bone density assessment, and varying degrees of artifact expression from patient motion and dense restorative materials, the authors noted.
However, strategies for reducing motion artifacts can be used, such as advising patients who are stressed or moving to close their eyes or adjusting the field-of-view during scout viewing prior to scanning to avoid acquisition of metal-containing areas that are not diagnostically useful, they explained.
Intraoral 3D scanners can provide greater accuracy than CBCT and greater comfort and efficiency than conventional impression-taking, and images can be combined with CBCT data. The technology allowing the creation of virtual models continues to develop, while 3D facial scanning can now be performed with some CBCT units. At the same time, poor image resolution can result in insufficient image quality and 3D model inaccuracy, Jacobs and colleagues wrote.
Standardization needed
Greater development of the virtual patient concept demonstrates the need for standardization of image data formats, they wrote. Additionally, CBCT may not be an ideal diagnostic tool after implant placement, although with technological advances, it could be useful for 3D imaging of peri-implant bone.
For now, CBCT appears helpful for the following postimplant situations:
- Postsurgical complications, such as neurovascular trauma
- Follow-up of healing from complex surgical procedures
- Maxillofacial trauma with suspected complications at the implant level
- Retrieval of osseointegrated implants in cases with infectious or mechanical failure etiology
"The variation in CBCT performances related to radiation doses and image quality emphasizes the need for more research to establish proper solutions for three-dimensional imaging following the ALADA (as low as diagnostically acceptable) principle, whilst focusing on artifact reduction caused by motion and metal," the authors concluded.