A teen in Canada developed the rare, life-threatening Lemierre syndrome, or the "forgotten disease," following sepsis from mandibular osteomyelitis after third-molar extractions. The case report was published in Oral and Maxillofacial Surgery Cases.
It is believed to be the first reported case of a healthy adolescent who underwent uncomplicated third-molar extraction and subsequently developed mandibular osteomyelitis from the bacteria Moraxella osloensis and Lemierre's syndrome, a rare condition that involves septic thrombophlebitis of the internal jugular vein. The 17-year-old boy made a full recovery after being treated with urgent operative debridement, antibiotics, and anticoagulant therapy, the authors wrote.
"Clinicians should be aware that Lemierre's syndrome can complicate mandibular osteomyelitis," wrote the authors, led by Dr. Dale Podolsky, PhD, of the Posluns Center for Image Guided Innovation and Therapeutic Intervention in Toronto (Oral Maxillofac Surg Cases, February 13, 2025).
A healthy 17-year-old boy with third-molar extractions
Initially, a healthy 17-year-old male had an unremarkable postoperative course after having his third molars extracted by an oral maxillofacial surgeon in the community. About six weeks after the extractions, he went to a clinic for worsening left-sided facial swelling and pain. He was given antibiotics for a suspected postoperative infection, the authors wrote.
Due to ongoing facial swelling and significant pain that persisted three months after the procedure, he went to a hospital emergency room. An x-ray revealed a patchy density throughout the left hemimandible, and a computed tomography (CT) scan was consistent with osteomyelitis of the left mandible with elevated inflammatory markers, they wrote.
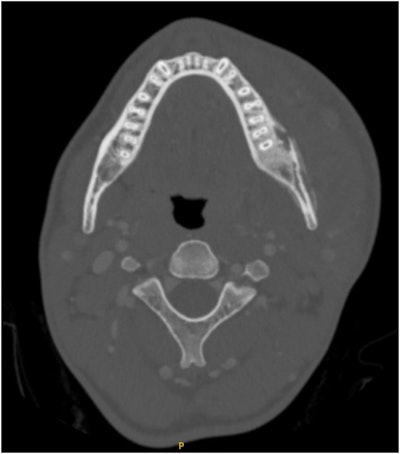 Axial CT scan demonstrating severe left hemimandible osteomyelitis with medullary and cortical osteolytic destruction and sclerosis with small abscesses on the buccal side of the mandible. Evidence of left masseter myositis and significant swelling of the masticator and left lingual space. Images courtesy of Podolsky et al. Licensed under CC BY-NC-ND 4.0.
Axial CT scan demonstrating severe left hemimandible osteomyelitis with medullary and cortical osteolytic destruction and sclerosis with small abscesses on the buccal side of the mandible. Evidence of left masseter myositis and significant swelling of the masticator and left lingual space. Images courtesy of Podolsky et al. Licensed under CC BY-NC-ND 4.0.
A day later, he was admitted to the hospital for ongoing pain and fever. Blood tests showed growth of Moraxella osloensis, and the boy was persistently febrile and tachycardic with signs of sepsis. He was given IV antibiotics.
Another CT scan revealed progression of the osteomyelitis, with new development of small abscesses on the buccal surface of the lower jaw. Also, there was an internal jugular vein left occlusion that clinicians believed was septic emboli or Lemierre syndrome, the authors wrote.
The boy underwent urgent debridement and was transferred to the postanesthesia care unit without issues. Also, he was given IV heparin. On the second day after the debridement, he was afebrile, and his pain and swelling had improved.
 Intraoperative view through the left Risdon approach demonstrating cortical erosion and scleroses of the buccal plate of the left mandibular body, angle, and ramus prior to debridement.
Intraoperative view through the left Risdon approach demonstrating cortical erosion and scleroses of the buccal plate of the left mandibular body, angle, and ramus prior to debridement.
However, an ultrasound of the patient's neck showed no flow in the left internal jugular vein, which was consistent with thrombophlebitis. The patient was transitioned from heparin to subcutaneous tinzaparin, they wrote.
Biopsy cultures revealed Streptococcus anginosus. Given the presence of septic thrombophlebitis and bacteria in keeping with Lemierre's syndrome, the patient was given peripherally inserted central catheter-line long-term IV antibiotics. The patient was discharged with antibiotics and anticoagulants after nine days in the hospital.
Six weeks postoperatively, an ultrasound showed resolution of the previous thrombus. However, severe narrowing of the internal jugular vein persisted. As a result, the patient remained on antibiotics for months, the authors wrote.
Unusual presentation
Lemierre syndrome has been described as a complication of bacterial throat infections, including tonsillitis, that leads to septic thrombophlebitis of the internal jugular vein. The syndrome has been linked to Streptococcus, Bacteriodes, Staphylococcus aureus, Klebsiella pneumonia, and most commonly Fusobacterium necrophorum. This is the first reported case of Lemierre's syndrome linked to Moraxella osloensis.
"This is the first known case of osteomyelitis-associated Lemierre's syndrome following uncomplicated third molar extraction in a healthy young adult with Moraxella osloensis," Podolsky and colleagues wrote.




















