Flapless implant surgery may appeal to dentists who would like to add implants to their practice but hesitate because of the surgical complexity involved. Research has shown that results with this approach can be as good as or better than conventional implants.
"With a little common sense and awareness of anatomy, it's a very safe procedure," William Becker, D.D.S., M.S.D., an associate professor of periodontology at the University of Southern California, told Dr. Bicuspid.com.
“With a little common sense and awareness of anatomy, it's a very safe procedure.”
— William Becker, D.D.S., M.S.D.
In a multicenter study published in the Journal of Periodontology (February 2009, Vol. 80:2, pp. 347-352), Dr. Becker and colleagues from Sahlgrenska Academy at the University of Gothenburg, the Hebrew University, the University of Washington, and private practice reported that flapless implant placement can result in less bleeding and minimized crestal bone loss, but with survival rates comparable to conventional implant placement.
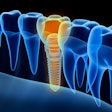
In traditional implant surgery, an incision is made in the gumline, and the flesh is peeled back to expose the bone crest and other underlying anatomy to see the bone and avoid perforating it or damaging other underlying anatomical structures.
As with traditional implants with flaps, flapless implants can be placed either where a tooth has been just pulled or where there hasn't been a tooth for a long time, if ever. Dr. Becker and his colleagues placed the implants at sites with no teeth.
The prospective clinical trial involved 79 implants in 57 adult patients from three clinical sites in the U.S., Sweden, and Israel. To be included in the study, patients had to have crestal bone width of at least 4 mm and vertical bone height (from the bone crest to the top of the mandibular canal or maxillary sinus) of at least 12 mm. They also had to agree to one-year follow-up.
Prior to treatment, the researchers took panoramic and periapical films of the proposed sites and used linear tomograms to measure crestal bone width and the distance to the floor of the maxillary sinus or top of the mandibular canal. They used surgical guides at most sites and precision drills with markings at 7, 10, 13, and 15 mm to drill through the mucosa and into the bone.
Next, the researchers measured from the mucosal margin to the bone crest to determine the appropriate osteotomy depth and implant length. They added this measurement to the planned implant depth from the tomogram. For example, if the bone depth was 10 mm and the mucosal measurement was 3 mm, they used the 13-mm line on the guiding drill.
The researchers placed the implants without water irrigation to a minimum torque of 30 Ncm. They placed healing abutments into the implants, following up weekly for four weeks, then again at an average of three years, eight months.
High success rate
After approximately four years, 37 patients with 52 implants were located for follow-up. Researchers acknowledged the high rate of participant dropout in the long-term trial and also the lack of a control group. Of the 52 implants, there was loss of only one, for a success rate of 98% in the implants reviewed.

Because no incisional healing was needed at the access flap site, there was less bleeding, the researchers noted. Other studies of flapless implants have shown there to be less pain and swelling, shorter surgery and recovery time, and less gum recession, leading to a better aesthetic effect and greater patient satisfaction (Practical Procedures and Aesthetic Dentistry, November/December 2008, Vol. 20:10, pp. 633-639).
But the approach doesn't fit all situations, said Kim Gowey, D.D.S., past president of the American Academy of Implant Dentistry. He has been doing implant surgery with and without reflected flaps for many years and sees pros and cons to flapless procedures.
"It doesn't work for all situations, as you cannot see the bone and can perforate or fenestrate the bone inadvertently," he said.
He recommends using cone-beam CT to visualize the bone, minimizing the risk of perforation and lowering the radiation exposure compared to conventional CT.
But Dr. Becker believes CT scans are overused, although he acknowledges that some states' guidelines may emphasize their use. CT scans can be "very good if you suspect the jaw may be too narrow, not only for the flapless but for a traditional approach," he said.
Some general dentists already perform flapless surgery in other circumstances, such as when they use guides and CT scans to drill through the gum tissue to place dentures in an edentulous arch, Dr. Gowey pointed out. But many dentists have done very little surgery, he noted.
"Some general dentists don't even take out third molars, but they get involved in implant surgery," he said. "Not having much surgical proficiency I'm sure increases the risk."
Experience required
The primary concern among dentists regarding flapless implants appears to be the risk of perforating or fenestrating the bone. Dr. Gowey thinks this can be more common if following the route of an extracted tooth. The drilled hole for an implant often needs to be more palatally placed than the natural hole left by the extraction, he noted.
"Someone inexperienced in surgery and not using CT increases the risk of complications related to perforating bone," Dr. Gowey said.
He often does what he calls a "miniflap" procedure for single implants, in which he makes an incision and peels back the tissue only enough to visualize the crest of the bone. This allows him to start in the right place, he explained, and also allows for only two sutures, one on each side of the implant.
Dr. Becker and Dr. Gowey agree that flapless implant surgery is only appropriate for implant surgeries where the patient has adequate bone width and height and adequate attached gingival tissue. They also agree that general dentists should become very comfortable doing implants with reflected flaps -- successfully performing at least 10 to 15 procedures, according to Dr. Becker -- before moving on to flapless implant surgeries.
Dr. Becker also emphasized the need for dentists to be very familiar with the anatomy of the maxillary and mandibular jaw, and to know about diagnosis and treatment planning.
"I lecture frequently, and I've encountered resistance from some of my close friends and colleagues who say that it's a dangerous procedure, but it's actually so simple," he said.
Copyright © 2009 DrBicuspid.com