A young woman experienced rare, life-threatening episodes of mouth bleeding for weeks following the uncovering of a dental implant. Details of the case were published on May 11 in Clinical Implant Dentistry and Related Research.
Clinicians managed the patient's bleeding by embolizing her descending palatine artery, which supplies blood to the hard and soft palate. It is possible that tooth loss changed the morphology of the patient's blood vessel anatomy.
Dentists should be aware that patients with tooth loss may experience delayed, uncommon bleeding, the authors wrote.
This is a "very rare case of a delayed episode of postoperative intraoral life-threatening hemorrhage in the maxillary region," wrote the group, led by Dr. Marco Dalle Carbonare of King's College Hospital National Health Service (NHS) Trust in London.
An unusual complication
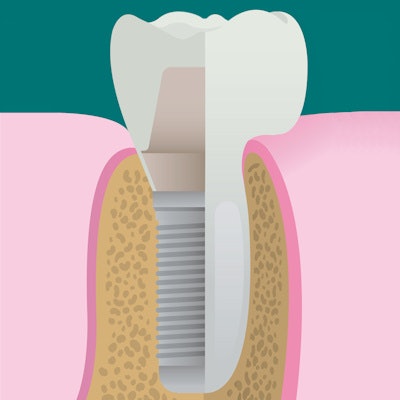
Postoperative bleeding associated with implant surgery typically is a minor, infrequent complication. In most cases, the bleeding is easily controlled. Though preoperative planning can minimize complications, unexpected and serious problems may occur.
Hemorrhage during implant placements is unusual, but when it does happen, it often occurs during the procedure or up to seven hours after the surgery. In previous cases, when the bleeding occurred, it was in the anterior upper jaw and was due to damage to the sublingual or submental artery. In the current case, this did not occur, the authors wrote.
The woman visited an emergency department after experiencing more than 40 bleeding episodes, including three significant events of intraoral bleeding, for two weeks following the uncovering of a dental implant on her upper right side. During minor episodes, methods such as localized pressure with gauze, use of local anesthetic with adrenaline, and suturing of the peri-implant gum temporarily stopped the bleeding for a maximum period of six days, the authors wrote.
Four months prior, the woman had a sinus lift surgery and an implant placed. She had juvenile periodontitis and hypodontia but no other health conditions.
While at the hospital, the woman's blood pressure dropped from 115/70 mmHg to 60/40 mmHg and her heart rate fell from 160 beats per minute to 60 beats per minute. Her hemoglobin was 74 g/L, which was an estimated blood loss of 1.5/2 L. She was deteriorating rapidly, so she was given four units of blood and two units of plasma, the authors wrote.
After the transfusion, the patient underwent computed tomography angiography, which revealed no active bleeding. After 24 hours, digital subtraction angiography (DSA) of the right external carotid artery showed no bleeding or vascular malformation. Clinicians applied fibrin sealant distal to the implant, with suturing of the gingival flap, and another cover plate was fitted.
Five days later, she went to the hospital again and DSA revealed a morphology change in the greater descending palatine artery with intra-alveolar vessels located close to the implant. Embolization of the artery was planned.
On the morning of the planned embolization, the woman experienced her third episode of significant bleeding. She underwent the embolization successfully. The woman has not had a bleeding episode in seven months since her artery was embolized. Clinicians continue to monitor her.
Due to localized juvenile periodontitis, the woman had tooth loss in all four quadrants of her mouth. Her tooth loss may explain the morphologic change in her palatine artery. Previous research suggested that dentition loss causes changes in vascular anatomy, according to the authors.
"Beware of delayed complications, uncommon bleeding sites (e.g., the maxilla), and potential anatomical variations following tooth loss," Carbonare and colleagues wrote.




















