Wearing overdentures supported by narrow-diameter implants can be an intriguing choice for older patients whose needs aren't met by conventional dentures but who require treatment that isn't too invasive. Because the long-term quality-of-life benefits of this option are unknown, investigators took a closer look.
They studied the oral health-related quality of life over a five-year period for patients who received overdentures after wearing complete dentures. The group found statistically significant improvements throughout the study, although these gains became less pronounced over time. The results were published May 28 in the Journal of Dentistry.
"The provision of four narrow-diameter implants in the edentulous mandible is a promising treatment option for patients with substantial oral health-related quality-of-life impairment and a positive attitude toward implant treatment," the authors wrote.
They were led by Daniel Reissmann, PhD, DMD, DDS, from University Medical Center Hamburg-Eppendorf in Hamburg, Germany, and Norbert Enkling from the University of Bonn in Germany and the University of Bern in Switzerland.
Give me five
Oral health-related quality of life is much lower in patients who wear conventional complete dentures than in those who have their own teeth, according to previous studies. Wearing complete dentures may cause discomfort, a lack of tactile sensitivity, foreign body sensation, and insufficient restoration of chewing function, especially in those with greater alveolar bone atrophy or higher needs for denture stability.
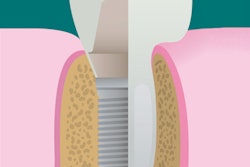
However, one option for edentulous patients is support of complete dentures with one or more implants in the mandibular midline. At the same time, such patients can be older, have comorbidities, use medications, and have overall reduced health, making such treatment disadvantageous because of a limited survival rate and high aftercare needs for such implants. Narrow dental implants with diameters of less than 3 mm present a promising alternative in such cases, the authors wrote.
"This approach allows placing implants in the alveolar bone in many cases with marked horizontal ridge atrophy without the need for augmentation procedures and without raising a flap," they explained.
“Improvement in oral health-related quality of life was substantial and clinically relevant.”
An International Team for Implantology consensus statement recommends placing four of these one-piece implants in the interforaminal region. Placement of narrow-diameter implants substantially improves oral health-related quality of life, according to previous research, but this has not been studied in the published literature beyond two years.
Therefore, the investigators prospectively studied oral health-related changes in quality of life over a five-year period in 20 consecutive patients treated with narrow-diameter implants at the University of Bern. The patients were edentulous for at least six months and wore complete dentures for at least 12 weeks. They ranged in age from 41 to 87 years, with a mean age of 66.9 years.
The researchers required that participants were living independently, were in good general health, and had interforaminal bone with a minimum width of 4 mm to 5 mm and a minimum height of approximately 13 mm. Exclusion criteria were the use of bone-altering medication(s), having dental anxiety, or abusing drugs.
Each participant underwent implantation with four one-piece titanium narrow-diameter implants that were 1.8 mm in diameter and 13 or 15 mm long (ESPE MDI mini dental implants, 3M). The researchers then measured how the patients assessed their oral health-related quality of life using the 49-item Oral Health Impact Profile (OHIP). The survey was administered at follow-up points up to five years after treatment.
The questionnaire asked whether various factors had affected their oral health-related quality of life during the past month, using a scale that ranged from 0 (never) to 4 (very often). Higher scores indicated more problems and lower oral health-related quality of life.
| Effect of narrow-diameter implants on oral health quality of life | |||||||
| Baseline (n = 18) | 4 weeks (n = 18) | 8 weeks (n = 18) | 12 months (n = 15) | 3 years (n = 19) | 5 years (n = 17) | p-value | |
| Oral function | 11.1 | 5.1 | 4.6 | 3.3 | 4.9 | 5.9 | < 0.01 |
| Orofacial pain | 6.3 | 4.5 | 2.8 | 2.0 | 3.9 | 4.2 | 0.006 |
| Orofacial appearance | 3.5 | 1.4 | 1.8 | 1.1 | 1.7 | 2.8 | 0.017 |
| Psychosocial impact | 9.4 | 6.1 | 5.4 | 6.7 | 7.0 | 8.9 | 0.086 |
| OHIP summary score | 38.9 | 21.8 | 18.2 | 15.9 | 21.7 | 26.5 | < 0.001 |
Oral health-related quality of life was substantially impaired in the study participants at baseline, with a mean OHIP summary score of 38.9. The score dropped to 21.8 four weeks after treatment and remained substantially lower through the final follow-up visit at five years. The summary and domain scores increased from the six-month and 12-month visits but never deteriorated to pretreatment levels.
Oral function experienced the largest changes during the study, while orofacial pain and orofacial appearance had moderate changes and psychosocial impact had the smallest changes.
"Improvement in oral health-related quality of life was substantial and clinically relevant, and lasted over the entire study period," the authors wrote.
They noted that OHIP summary scores after treatment were substantially lower than those of patients with new conventional complete dentures. In addition, the treatment-induced drop in the score lasted longer than has been reported for conventional complete dentures. They explained that the support of the implants may stabilize the denture, improve biting and chewing ability, and reduce sore spots.
Small sample
The small sample size of the study limited its statistical power, the authors noted. Additionally, treatment was not randomly assigned, and the study did not have a control group.
Despite these drawbacks, the study's findings have important clinical implications, the authors concluded.
"Patients can be informed in the decision-making process that treatment-related improvements in oral health-related quality of life are expected to last substantially longer than for conventional complete dentures," they wrote. "However, whether implant placement is also beneficial for patients coping very well with their complete dentures is not clear so far."