Thinking about adding silver diamine fluoride (SDF) to your caries treatment tool kit? A family dentist told a packed room at the recent 2017 ADA annual meeting in Atlanta that SDF needs the same thoughtful use and treatment planning as you would deliver with any treatment.
 Brooke Fukuoka, DMD.
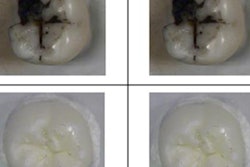
Brooke Fukuoka, DMD.Brooke Fukuoka, DMD, who owns a practice in Twin Falls, ID, serving adults with special needs, spoke about SDF, which has been used for decades in some countries, including Japan, Australia, China and Brazil, but is only more recently becoming more well-known in the U.S. Fairly simple to apply, the noninvasive treatment has the drawback of black staining.
"We can't just go slapping it all over everybody because it seems like a miracle cure," she told DrBicuspid.com after her presentation. "It does have to be treatment planned and well thought out."
Gaining acceptance
In 2014, the U.S. Food and Drug Administration (FDA) approved the use of SDF for desensitization. Advantage Arrest silver diamine fluoride 38% (Elevate Oral Care) became available in the U.S. in 2015.
The following year, the Journal of the California Dental Association published the University of California, San Francisco protocol for SDF use for caries arrest, which recommends SDF application twice a year to carious lesions without excavation for at least the first two years. Additionally, an article about the use of SDF in kids published in the New York Times (July 11, 2016) brought significant attention to the treatment, Dr. Fukuoka noted.
Meanwhile, the American Academy of Pediatric Dentistry conditionally recommended the use of SDF as a topical treatment for cavities in pediatric patients in October 2017.
Who can apply it? That varies by state, especially for dental hygienists and assistants, although in some states its use has not been addressed at all, Dr. Fukuoka explained. Even though it is not varnish, SDF is sometimes treated as varnish under regulations in some states, she said.
It is currently being used at locations in the U.S., including UCSF, the University of Washington, and various community health centers and pediatric practices, Dr. Fukuoka noted.
When to use it
The use of SDF is appropriate only in certain situations, according to Dr. Fukuoka.
"When aesthetics are not an issue," she said. "It's not a very pretty treatment."
She noted some types of patients and dental situations in which SDF can be helpful:
“We can't just go slapping it all over everybody because it seems like a miracle cure.”
- Small children who can avoid sedation, drilling, or filling and be kept out of the operating room
- Patients who are noncompliant with oral hygiene
- Patients with special needs
- Patients whose caries can't all be fixed in one visit but who would benefit from their arrest, such as those with "meth mouth" or who have made poor decisions
- Nonrestorable endodontically treated teeth to help patients live with what they have when they don't have a way to get something new
- Questionably restorable teeth
- Difficult-to-reach furcations
- Recurrent caries on extensive prosthodontic work
- Prolonging the use of a poor prosthodontic bridge
However, SDF should be avoided in some situations and patients, such as the following:
- When aesthetic concerns outweigh the potential benefits
- Patients who are allergic to silver
- In the presence of open soft-tissue lesions
- Pregnant patients
Dr. Fukuoka advised dental practitioners to figure out for which patients SDF is best and noted that the results of joint decision-making might not be what they expect.
"We're not just treating caries, we're treating patients," she said.
Dr. Fukuoka shared an anecdote about a patient with autism who skis in the Special Olympics who didn't always remember to brush and experienced tooth sensitivity while skiing. After she applied SDF on his teeth, he was delighted with the black color since it reminded him to brush when he saw it.
"Don't be afraid of the black," she said.
Dr. Fukuoka mentioned the results of a recent study on parental acceptance of SDF (Journal of the American Dental Association, July 2017, Vol. 148:7, pp. 510-518.e4). When surveyed, 67.5% of the parents were OK with the use of SDF on their children's posterior teeth, while 29.7% of the parents approved of it for anterior teeth. In addition, as the number of behavioral barriers to conventional restorations in the children and the need for general anesthesia for treatment increased, so did the parents' acceptance of SDF.
Dr. Fukuoka's protocol in her practice with special needs patients calls for SDF treatment to be repeated every three months for the first year and every six months after that if the lesion remains hard. Although it does arrest decay, it does not fill cavitations, she said.
"It's a very easy treatment, but it's also not a treatment that doesn't have potential ramifications," she concluded.