How prevalent is peri-implant disease? And what are its pathogenesis and risk factors, as well as the best ways to diagnosis and treat it? An expert on inflammation and regeneration offered practical device on the changing facets of this increasingly common condition.
 Mark Reynolds, DDS, PhD, spoke on peri-implant disease.
Mark Reynolds, DDS, PhD, spoke on peri-implant disease.Mark Reynolds, DDS, PhD, a professor and dean of the University of Maryland School of Dentistry in Baltimore, spoke to DrBicuspid.com after his presentation at the recent California Dental Association's CDA Presents 2017 meeting in San Francisco about how peri-implant disease has been changing over time. He is the author of numerous peer-reviewed articles on inflammation and regeneration.
"Peri-implant disease is more prevalent than most practitioners recognize," Dr. Reynolds said. "Early treatable inflammation associated with peri-implantitis should not be overlooked given that it could progress to peri-implantitis."
Population changes
Dental implants are becoming more common, although the magnitude of the change in peri-implant disease is unknown, Dr. Reynolds said.
Peri-implant mucositis is found in 43% of implants and peri-implantitis in 22%, according to information from a study he mentioned during his presentation (Journal of Clinical Periodontology, April 2015, Vol. 42:suppl 16, pp. S152-S157). Bleeding on probing is a key way to distinguish between peri-implant health and disease, while a lack of regular supportive therapy in peri-implant mucositis is associated with greater risk of peri-implantitis, according to the study, which was based on the results of a working group informed by four systematic reviews on peri-implant disease epidemiology.
“Early treatable inflammation associated with peri-implantitis should not be overlooked given that it could progress to peri-implantitis.”
However, about 10% of implants will have peri-implantitis after five to 10 years in 19% of patients, according to another systematic review and meta-analysis (Journal of Periodontology, November 2013, Vol. 84:11, pp. 1586-1598) Dr. Reynolds discussed. Mucositis was found in 31% of implants and 63% of patients. At the same time, another study reported substantially lower numbers.
He also spoke about shifts in the prevalence of health factors that affect peri-implant disease. Demographics are changing and so are risk factors for peri-implantitis and other oral health diseases, Dr. Reynolds noted.
"The public is changing," he said. "We are taking out teeth in young adults related to substance abuse."
These evolving public health factors include the reduction in cigarette smoking, increase in diabetes, and the epidemic of substance abuse. Other emerging issues, such as increasing depression, stress, and anxiety, also are having an effect, Dr. Reynolds said. However, to understand the true prevalence of peri-implant disease, a large number of patients would need to be studied.
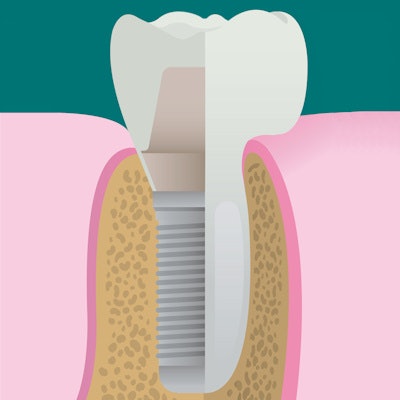
Additionally, the continual evolution of implant designs can make studying implants difficult, he said, but there doesn't appear to be a significant difference in prevalence of peri-implantitis between tuned and moderately roughened implants.
"Our surgical technique has not really changed appreciably, although the ability of implants to integrate has improved," he said.
Risk factors
Peri-implant disease is common and can happen even when patients are treated by well-trained practitioners, Dr. Reynolds said during his lecture. Healthy patients, however, experience less bone loss, a lower incidence of peri-implantitis, and better implant success, according to the results of multiple studies.
Previous periodontal disease is a key risk factor for peri-implantitis because of bacterial flora, but implant survival has not been found to be affected by it, he said.
"The same pathogens are associated with both implant disease and susceptible teeth," Dr. Reynolds said.
In addition, poor plaque control or the inability to clean implants well can increase the risk for peri-implant disease. Implants, themselves, can make adequate home care, clinical evaluation, and professional debridement difficult, he noted. Smoking, excess cement, and lack of supportive therapy also increase peri-implant disease risk. Five-year follow-up has found 2.5 times the rate of peri-implantitis in patients without maintenance.
Studies examining the relationship of diabetes, occlusal overload, or genetic factors to peri-implant disease have not reached definitive conclusions.
Identify problems early
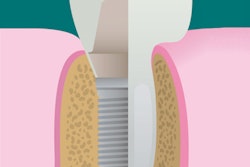
Flagging problems earlier can be helpful. Signs of peri-implant mucositis include bleeding on probing and/or suppuration, which are usually associated probing depths of 4 mm or greater and no evidence of radiographic bone loss beyond bone remodeling.
Unfortunately, evidence-based information on treating peri-implantitis is lacking.
"It's clinical judgment and experience," Dr. Reynolds said.
There's a lot of interest in understanding how to manage peri-implantitis nonsurgically, he said, although the comparative effectiveness of various nonsurgical treatments for peri-implantitis remains unclear.
Dr. Reynolds discussed a review study that found insufficient evidence that nonsurgical treatments, such as debridement in conjunction with antibiotics, PerioChip, or photodynamic therapy, were superior to debridement alone (J Clin Periodontol, October 2014, Vol. 41:10, pp. 1015-1025).
The literature is fairly consistent in saying that systemic antibiotics don't work, Dr. Reynolds said. Bacteria live in biofilms and antibiotics often are not effective at reaching dental infections.
Implant removal, lesion treatment, and implant resection are treatment options. The degree of bone loss can affect whether implants can stay in.
"Most people are in agreement that once you hit the 50% mark, the implants are going to come out," Dr. Reynolds said.