Cat's claw, or Uncaria tomentosa, is a plant that is used to improve various symptoms associated with osteoarthritis and rheumatoid arthritis. But does it have the potential to treat denture stomatitis?
Denture stomatitis affects many denture prostheses wearers, including up to 65% of the elderly who rely on total dentures, according Brazilian researchers from Ponta Grossa State University, the University of Estadual Paulista, and the University of Campinas (Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, July 2014, Vol. 118:1, pp. 72-77). Pain, irritation, and salivary disruption are all common symptoms, but it is also possible not to have an inflammatory reaction at all, so some patients are unaware that they have the condition.
Treatment usually involves topical or systemic antifungal medications. Recent research, however, has focused on the effectiveness of phytotherapeutic agents, which are derived exclusively with plants or parts of medicinal plants. They are less costly, are less toxic, and have fewer side effects than many synthetics, according to the study authors. But few studies have looked at the possibility of using cat's claw, which has an established reputation for being effective against arthritis-related inflammation, based on the results of in vitro and in vivo studies.
“U. tomentosa, as an herbal treatment, might be more economical than other treatments for patients.”
In a double-blind study, the researchers sought to test the ability of a U. tomentosa gel to reduce infection in the denture-supporting tissues of patients with denture stomatitis. They found that it "was an effective topical adjuvant treatment" and "it had the same effect as 2% miconazole gel." In addition, "U. tomentosa, as an herbal treatment, might be more economical than other treatments for patients," they noted.
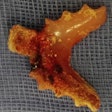
The researchers recruited 50 participants who were between the ages of 45 and 85, had worn dentures for at least one year, and had denture stomatitis type I, II, or III based on Newton's criteria. Individuals with type I have bleeding spots; those with type II have diffuse erythematous areas; and those with type III have granular inflammation. Reasons for exclusion in the study included having xerostomia, diabetes, recent treatment involving antibiotics, or poorly fitting dentures.
Once selected, the participants were examined by the researchers to learn about their oral health, the presence of oral lesions, and the condition of their dentures. The researchers took microbiologic cultures from the palatal mucosa and surface of the dentures to identify candidiasis, a fungal infection most often responsible for denture stomatitis.
Next, the 50 patients who met the researchers' criteria were randomly divided into one of three experimental groups:
- Group M served as the positive control, and 13 were given Daktarin gel (Janssen-Cilag), a 2% miconazole gel.
- Group P served at the placebo group, and 16 were given 1.5% Natrosol (Fleming Manipulações), or hydroxyethyl cellulose.
- Group UT served as the experimental group, and 17 were given 2% U. tomentosa gel (Fleming Manipulações).
Each was instructed to clean their dentures and apply 2.5 mL of the gel they received at the base of the denture after eating, three times per day for one week. They were not worn at night. Forty-eight participants finished the study.
Examinations by the researchers took place on day 0, at the end of the treatment period on day 7, and one week afterward, or day 14. During these visits, the researchers made observations of the palatal mucosa and asked the subjects about any irritation, burning, nausea, vomiting, or diarrhea they experienced. They also took images of the mucosa, which were blindly analyzed by two independent calibrated dentists. In addition, the researchers swabbed the palatal mucosa and tissue surface of the upper denture to recover Candida and determine the number of colony-forming units per milliliter (CFU/mL). Lastly, they analyzed their results to measure the effectiveness of each treatment.
The severity of denture stomatitis actually diminished over the evaluation periods with no significant differences among the treatments (p > 0.05). "Thus, it is not possible to affirm that the U. tomentosa gel was solely responsible for this reduction," the researchers explained. "The reduction of fungal load from dentures and palates after treatments, associated with patients' compliance with the oral denture hygiene (including denture removal during sleep), might be responsible for the observed effect."
However, the researchers believed that U. tomentosa could be used as an alternative denture stomatitis treatment, and they agreed with the findings of previous research with similar conclusions. Also significant, some clinical isolates have proved resistant to miconazole's scientifically proven ability to act as an antifungal, the researchers noted.
"The use of alternative treatments such as phytotherapeutic agents is promising," they wrote. "U. tomentosa gel is an effective topical adjuvant treatment for denture stomatitis." Treatment of one week with the gel was sufficient to be effective, but its use must be associated with hygiene methods for a successful treatment, they concluded.