A woman in Japan can once again feel pain and temperature in her mouth thanks to the immediate repair of her alveolar nerve, which was damaged during jaw surgery. The case report was published on May 10 in the Journal of Oral and Maxillofacial Surgery, Medicine, and Pathology.
Clinicians cut her inferior alveolar nerve, which supplies sensation to the lower teeth, while performing a bilateral sagittal split ramus osteotomy to align the woman's jaw. This is believed to be the first report to evaluate neurosensory disturbance after immediate repair of this severed dental nerve using a polyglycolic acid sheet and stellate ganglion block. The woman's mouth sensations were restored after 15 months, the authors wrote.
 Intraoperative view of the patient's mouth. (A, B) The white arrow points to the severed inferior alveolar nerve (IAN). (C) The nerve was removed from the mandibular foramen. All images courtesy of Kasahara et al. Licensed under CC BY-NC 4.0.
Intraoperative view of the patient's mouth. (A, B) The white arrow points to the severed inferior alveolar nerve (IAN). (C) The nerve was removed from the mandibular foramen. All images courtesy of Kasahara et al. Licensed under CC BY-NC 4.0."The paresthesia in right sensory domain of the IAN [inferior alveolar nerve] had been restored to that before the surgery," wrote the group, led by Dr. Kiyohiro Kasahara of the department of oral pathobiological science and surgery at Tokyo Dental College.
A bilateral sagittal split osteotomy is a type of jaw surgery in which the lower jaw is moved forward or backward to improve teeth alignment. Fractures, excessive bleeding, and damage to the inferior alveolar nerve or lingual nerve are known risks associated with the procedure. Though nerve damage is a well-documented complication and medical professionals agree early nerve repair results in better outcomes, there is little evidence describing outcomes following immediate repair.
In August 2019, a woman was given general anesthesia and underwent a bilateral sagittal split osteotomy to treat her protruding lower jaw. During the procedure, surgeons confirmed that her inferior alveolar nerve was severed completely. They reorganized her treatment plan so the surgeons could repair the nerve immediately, the authors wrote.
 Intraoperative view after nerve repair. (A) The white arrow points to the three 7-0 polyglycolic acid sutures. (B) The white arrow points to the polyglycolic acid mesh sheet used to protect the repaired nerve. (C) A monocortical titanium plate with five screws was used for the repair.
Intraoperative view after nerve repair. (A) The white arrow points to the three 7-0 polyglycolic acid sutures. (B) The white arrow points to the polyglycolic acid mesh sheet used to protect the repaired nerve. (C) A monocortical titanium plate with five screws was used for the repair.First, supersonic wave instruments were used to remove the split osteotomy stump of the distal segment of the right side of the jaw. This provided a better view of the distal inferior alveolar nerve, which had been ripped from the lower jaw foramen, they wrote.
Next, clinicians sutured the nerve stump and removed the right distal part of the buccal cortical bone to get a better view of the proximal side of the nerve. Because moving the fixed jaw could cause the nerve reconnection to fail, they repaired the nerve before performing the intermaxillary fixation. They stitched up the epineurium every 120° using three polyglycolic acid sutures while using a magnifying glass. They protected the repaired portion with absorbable polyglycolic acid mesh sheet.
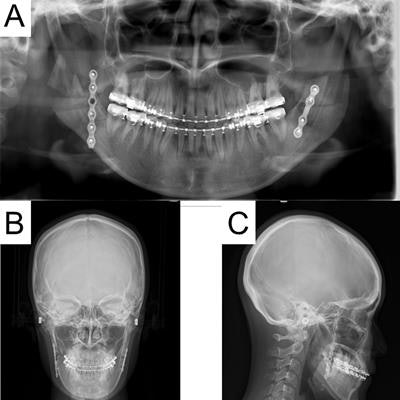
Finally, clinicians put back the removed distal cortical bone. A monocortical titanium plate with five screws was used to fix the right side, and a plate with four screws was used to fix the left side. Surgeons checked her mouth opening and occlusion after they removed the wires between her upper and lower jaws and then closed the wound. X-rays taken after the procedures showed no abnormalities.
 Postoperative radiographs of the patient showed no abnormalities.
Postoperative radiographs of the patient showed no abnormalities.Throughout the procedures, the woman was injected with numbing agent 27 times to minimize pain. She was prescribed 6.6 mg of dexamethasone sodium phosphate for 14 days and vitamin B12 for six months after surgery, the authors wrote.
Immediately after the surgeries, the woman's right dental nerve did not respond to pain or temperature. The perception of sensation was tested again at three months and at six months. She started feeling some sensation at six months and then continued to improve. Prompt treatment along with the use of the polyglycolic acid mesh sheet and stellate ganglion block aided in her recovery, the authors wrote.
"The sensations of pressure, pain, and temperature after one year and three months were restored to the preoperative level," Kasahara and colleagues wrote.