Maxillofacial surgeons who used CT intraoperatively on their trauma patients found that imaging and review can be performed quickly, perfecting the trauma surgeon's work while there's still time to make revisions, according to an article published this month in JAMA Facial Plastic Surgery.
A new analysis of intraoperative CT in 38 patients found that the total scan time of about 14 minutes did not differ significantly between routine and complex cases. However, intraoperative revisions were more common in complex (n = 8) than routine (n = 1) cases, suggesting that CT may be more helpful in difficult cases, the authors wrote (JAMA Facial Plast Surg, January 8, 2015).
 Dr. David Shaye from Massachusetts Eye and Ear Infirmary and Harvard Medical School.
Dr. David Shaye from Massachusetts Eye and Ear Infirmary and Harvard Medical School."We're starting to use [intraoperative CT] as another facet in the algorithm of how you treat trauma," said co-author David Shaye, MD, from Massachusetts Eye and Ear Infirmary, in an interview. "It gives you that added bonus that if you see anything, you can make some minor adjustments."
For example, say the surgeon is placing a mesh implant to reconstruct an orbital floor fracture, and he or she notices in the intraoperative CT images that the placement is slightly off. Maybe the contour of the orbit doesn't precisely mirror the other side of the face.
"If we get this information at the time of surgery when the incisions are all open, there's no reason you wouldn't adjust something" before closing the patient up, he said. Without intraoperative CT, a misalignment wouldn't be noticed until after surgery, and at that point only major problems are likely to lead to the patient being put under anesthesia again for corrections.
"It gives us this really valuable information intraoperatively," Dr. Shaye said of the technique. "You want to make sure all of this is very precise."
In the current study, Dr. Shaye and colleagues Travis Tollefson, MD, MPH, and Bradley Strong, MD, from the University of California, Davis, aimed to evaluate the time needed to perform intraoperative CT scans during maxillofacial surgery, as well as measure any trends toward shorter total scan time as surgeons gained experience with the technique. They also wanted to identify the characteristics of cases that required intraoperative revision. The study findings suggest, but do not yet prove, that the technique creates better outcomes.
"We were able to show that, first of all, intraoperative CT isn't too onerous," Dr. Shaye said. "Most people would dismiss [intraoperative CT] because they think it's going to add too much time to the case. But it's only 14 minutes added to the case. There's a little bit of a learning curve, but you can overcome that quickly, and we show some examples where you would make an adjustment [during surgery] based on the data."
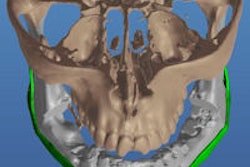
 An intraoperative portable CT scan is being performed after open reduction of a facial fracture. Upon satisfactory reduction, confirmed by the scan, incisions are closed and no further imaging is necessary. If the scan shows a need for modification of the reduction or facial implant, adjustments are made at that time. No postoperative imaging is required. All images courtesy of Dr. David Shaye.
An intraoperative portable CT scan is being performed after open reduction of a facial fracture. Upon satisfactory reduction, confirmed by the scan, incisions are closed and no further imaging is necessary. If the scan shows a need for modification of the reduction or facial implant, adjustments are made at that time. No postoperative imaging is required. All images courtesy of Dr. David Shaye.Between 2012 and 2014, the group performed 38 procedures at the two centers using intraoperative CT on 30 men (79%) and eight women (21%), who had a mean age of 37.4 years (± 16 years). Each case was labeled as routine or complex.
Portable scanners were used, along with MDCT, which provides the best image resolution, and cone-beam CT, which delivers exceptionally low radiation doses in the 40 µSv to 80 µSv range (versus 400 µSv to 800 µSv for MDCT).
Intraoperative CT became feasible with the advent of portable CT scanners, but the early models were cumbersome, offering only rudimentary segmentation and volume-rendering capabilities, the authors wrote. Current portable CT scanners have smaller footprints, greater maneuverability, better image resolution, and lower radiation exposure. As a result, they are becoming more common in intensive care units, emergency departments, and operating rooms.
In the study, surgeons notified the radiology department the morning of surgery, and the technologists warmed up the scanner and placed it just outside of the operating room prior to surgery. A C-arm drape was placed over the patient before the scanner was positioned over the patient's head, the authors explained. The scanner and drape were removed while the surgeons formatted and read the scans to prepare the patient for wound closure or revision, as indicated by imaging.
 Preoperative CT scan (above) shows a left-sided zygomaticomaxillary complex fracture that is moderately displaced and rotated. After sublabial access and mobilization, reduction is confirmed with intraoperative CT (below). Reduction has been achieved and no further incisions are necessary.
Preoperative CT scan (above) shows a left-sided zygomaticomaxillary complex fracture that is moderately displaced and rotated. After sublabial access and mobilization, reduction is confirmed with intraoperative CT (below). Reduction has been achieved and no further incisions are necessary.Mean total scanning time was 14.5 ± 4.9 minutes (range, 6-27 minutes) from start to finish, including draping and undraping the patient. A linear regression model was used to test the hypothesis that total scan times would decrease in the latter months of the two-year study; however, they did not appear to decrease.
A second linear regression model looked for differences in scan times between the more-experienced and less-experienced surgeons. Dr. Shaye and colleagues found that scan time for the most experienced surgeon was 3.78 minutes shorter than for the other surgeons as a group (p = 0.02). The day of the study had only an insignificant effect on these times, the authors wrote.
Complex cases
Among the 38 cases, 20 were noted as complex and 18 were routine. Intraoperative revisions were performed in nine (24%) of the 38 patients, and eight of these occurred in cases identified as complex, the researchers found.
The eight complex cases with intraoperative revisions included five orbital reconstructions, one panfacial fracture, two orbitozygomatic fractures, and one orbitozygomatic tumor reconstruction. Among the nine patients who had intraoperative revisions, three underwent repeat scanning to verify final placement of the implant, including two who were undergoing complicated secondary orbital reconstructions.
"Of the total scan time, the surgeon's role (patient preparation and scan interpretation) is quite brief," Dr. Shaye and colleagues wrote. "There is little room for improved efficiency; however, the technician's role (scanner positioning and data processing) is the most time-consuming and has the greatest potential for improved efficiency."
Like the experienced surgeons, the experienced CT technologists appeared to have the shortest scan times, although this anecdotal finding was not backed by data, the authors wrote.
The study showed that intraoperative CT is fast, and while imaging times did not decrease during the study, surgeons with more experience can be expected to perform faster. The authors recommended intraoperative CT imaging for maxillofacial reconstruction, especially in complex procedures.
And while presurgical imaging is the gold standard, postsurgical scans may or may not be necessary when there is intraoperative imaging, Dr. Shaye said. A lot of people want postsurgical images to see if they've reconstructed a complicated fracture adequately, but there is disagreement about the need for three scans.
"After the whole surgery's done, traditionally there's a subset of difficult fractures where the surgeon will have a CT done on the patient ... 'Where's the titanium, where are the plates, am I happy with the projection of the cheek?' and all sorts of things," he said. "If not, they'll go back into the operating room."
Without intraoperative CT, if the postsurgical period reveals something minor that needs adjusting, "you have to ask yourself, is it really worth opening everything up and going back to the operating room?" Dr. Shaye said. "Usually the answer is no unless something is grossly off."
"But we weren't able to show that [CT] makes revisions rarer," he noted. "You need a much bigger, broader study to show that."
Going forward, he wants to study how intraoperative CT can actually change the operative algorithm. Repairing a cheekbone fracture traditionally requires several entry points: one at the eye, one in the conjunctiva, one under the eyelid, and one under the lip.
"I think we could actually do fewer incisions -- just one underneath the lip, and it can be extremely small," he said.
Then the surgeon would move the bone and see if it settled into the right place. Surgery might not even be necessary half of the time, and it can be left to heal at that point. If that were the case, "I think that's worth a scan," Dr. Shaye said.