When a patient is rushed in with an injured tooth, what is the best approach to preserve the tooth's pulp, pulpal space, and root? DrBicuspid.com spoke with four endodontists on best practices in treating a patient in these circumstances. They recommend a team effort with general dentists and staff on the front line and endodontists joining in to preserve the tooth's pulp, pulpal space, and root.
When an endodontist is called in to help with trauma treatment, a number of considerations come into play, including injury stabilization, alveolar ridge preservation, bacterial complications, and healing potentials.
Injury stabilization
If the injury has loosened the tooth significantly, one of the first steps in treatment is stabilization, said Stephen Cohen, DDS, former chair of the endodontic department at the University of the Pacific Arthur A. Dugoni School of Dentistry and senior co-editor of the textbook Cohen's Pathways of the Pulp.
In stabilizing the tooth, "it's important that the tooth be allowed to move slightly," he noted. "If the tooth is made completely rigid, root resorption or the opposite, ankylosis, could occur. In ankylosis, the root is replaced by bone as a result of the periodontal ligament disappearing, so bone grows into the tooth, locking the tooth into the bone -- something that can be quite harmful to the growth and development of an adolescent."
Alveolar ridge preservation
"Alveolar ridge preservation is only a concern if the tooth is knocked out," said Alvin Arzt, DDS, a retired Pennsylvania dentist who is the founder and past president of the American Endodontic Society (AES).
"Alveolar bone supports the tooth. It's like the dirt around the roots of a tree," he said. "If the tooth can be replaced in the socket, the alveolar ridge will be preserved."
“The most common bacterial infection is infection of the root canal secondary to pulp necrosis.”
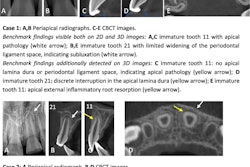
A wide variety of factors figures into healing potentials. In general, the two most important factors are the type of injury and the degree of root development, said Linda Levin, DDS, PhD, vice president of the American Association of Endodontists.
"We do not have sound statistics on the actual rate of infection, but we do know the incidence of pulp necrosis after certain injuries. It can be presumed that after pulp necrosis, infection follows," she said.
"A classic study on 400 patients with more than 600 luxated teeth followed over 10 years reveals that pulp necrosis is related mainly to the type of injury and the stage of root end development. Pulp necrosis and, therefore, infection increase with the extent of injury," Dr. Levin said, citing a 2006 study by Frances Andreasen, DDS, Dr Odont, and colleagues in Dental Traumatology (April 2006, Vol. 22:2, pp. 99-111).
"According to Frances Andreasen, concussion and subluxation represent the least risk, followed in ascending order by extrusive, lateral, and intrusive luxation," she said.
Bacterial complications
"The most common bacterial infection is infection of the root canal secondary to pulp necrosis," Dr. Levin said. "While soft-tissue infections can occur when foreign bodies or debris are in a wound, when they occur, it is shortly after the trauma."
On the other hand, "endodontics infections can occur anywhere from days to years after a trauma," she noted. "Once the pulp necroses, there is no longer vascular access for the host immune response," leaving the tooth without protection from bacterial invasion and resulting infection.
With this in mind, "if we see necrosis in the tooth, we treat it immediately" before it can progress to infection, Dr. Levin said. This is because once the pulp becomes necrotic, it's not a question of if the tooth will progress to infection, but when.
For this reason, "root canal therapy should be performed as soon as pulp necrosis is confirmed to avoid infection and inflammatory root resorption," she said.