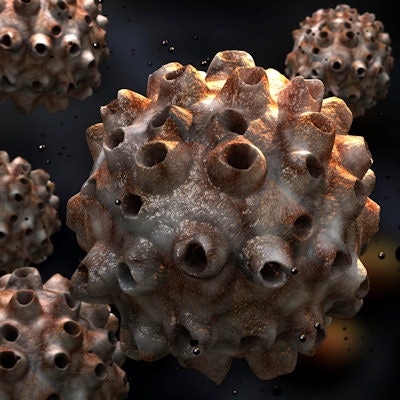
Time to have that talk? Dental practitioners are well-positioned to help patients prevent cancers related to human papilloma virus (HPV) but can find it difficult to communicate with them about the topic. A new study examined the role of practitioners in this area and what might help them do a better job.
Dentists and hygienists participated in focus groups and completed surveys about their roles and needs related to HPV prevention. They affirmed the importance of their participation in preventing HPV-related cancers, but they also reported that the practice environment, certain patient characteristics, and the topic's sensitivity can hamper communication efforts (Papillomavirus Research, March 7, 2018).
"Providers expressed concerns about how these conversations may affect their patients and practices due to the sensitive nature, yet they requested the materials and skill-building training to facilitate this process," the authors wrote.
The lead study author is Nolan Kline, PhD, MPH, formerly of the University of South Florida College of Public Health in Tampa and now an assistant professor of anthropology at Rollins College in Winter Park, FL.
Can we talk?
HPV is the most common sexually transmitted virus and infection in the U.S., and HPV-related oropharyngeal cancers are a growing public health concern. About 63% of oropharyngeal cancers are due to HPV and may be preventable, the authors noted. The HPV vaccine is licensed for males and females between the ages of 9 and 26 and recommended for 11- and 12-year-olds, although it is not yet approved for preventing HPV-related oropharyngeal cancers.
The ADA has recommended that dental practitioners educate themselves and their patients about the connection between HPV and oropharyngeal cancer. Previous research has found that dental patients could use more information on HPV and oral cancers, and the growing awareness of the HPV vaccine could lead more patients to ask about its role in oral cancer prevention.
“Dental providers may well become the next line of prevention of this rapidly increasing oral health concern.”
Since some dental providers already screen for oral cancer, they could expand this work to include education about HPV and prevention efforts, such as the HPV vaccine, but research indicates that many of them are not yet ready to do so. Therefore, the researchers conducted the current study to gain a greater understanding of dental providers' needs and perceived roles related to preventing HPV-related oropharyngeal cancer.
They organized four focus groups of dentists who attended a regional conference in the southeastern U.S. in 2016 and four focus groups of hygienists who attended a national U.S. conference in 2015. Each group consisted of eight to 10 dentists (n = 33) and 10 to 12 (n = 48) hygienists. Participants completed demographic questionnaires and discussed in the groups what they needed to facilitate discussion of HPV and oral cancer risks with their patients.
Additionally, 55 dentists and 228 hygienists who took part in continuing education (CE) sessions on HPV-related oropharyngeal cancer at the regional dental conference completed a survey about their roles and needs related to discussing HPV with their patients, as well as the barriers to and facilitators of doing this.
The researchers conducted preliminary interviews with key opinion leaders in the dental profession, which subsequently served to inform the survey questions and focus group guide.
The study participants affirmed a role for the dental profession in educating patients about HPV and screening them for HPV-related cancers. Hygienists described themselves as "prevention specialists" whose work encompassed education and screening. Dentists were generally more focused on oropharyngeal cancer prevention through oral cancer screening while recognizing a role for vaccine education and recommendation.
The participants also identified needs they wanted fulfilled to overcome barriers to providing HPV education to patients.
"The most salient discussion surrounded the need for patients, rather than providers, to begin conversations about HPV," the authors wrote. "Participants mentioned patient-initiated conversations would remove their concern of offending or embarrassing patients by bringing up a sensitive topic and would additionally signal to the provider that the patient is interested in learning more about HPV."
| Barriers to discussing HPV & oropharyngeal cancer | ||
| What would make it difficult for you to discuss the connection between HPV and oral cancer with your patients? | ||
| Barriers | Dentists (n = 37) |
Hygienists (n = 166) |
| Lack of privacy (e.g., open operatory) | 20 (54%) | 90 (54%) |
| Fear of offending patients | 19 (51%) | 98 (59%) |
| Patient population and demographics (e.g., age, gender) | 16 (43%) | 42 (25%) |
| Lack of time | 14 (38%) | 85 (51%) |
| Not knowing enough | 8 (22%) | 45 (27%) |
| Not feeling comfortable | 6 (16%) | 34 (21%) |
For dentists, the most common concerns were lack of privacy, fear of offending patients, and patient population and demographics, such as age and gender, while hygienists were most concerned with a fear of offending patients, lack of privacy, and lack of time.
Study participants cited three areas in which they thought increased attention would, in turn, help to improve their HPV prevention efforts:
- Greater patient awareness of HPV and oropharyngeal cancer to allow for patients to begin discussions on these topics
- More comprehensive, passive patient education materials on the relationship between HPV and oropharyngeal cancer to facilitate patients beginning the conversation
- Greater professional education about HPV that could be addressed through CE courses covering topics such as the relationship between HPV and oropharyngeal cancer and how to communicate with patients about related topics
| Facilitators to discussing HPV & oropharyngeal cancer | ||
| What would make it easier for you to discuss the connection between HPV and oral cancer with your patients? | ||
| Facilitators | Dentists (n = 37) |
Hygienists (n = 166) |
| Continuing education in journals | 35 (95%) | 139 (84%) |
| Waiting room pamphlets | 33 (89%) | 149 (90%) |
| Technology support materials (e.g., mobile apps, electronic health records) | 27 (73%) | 117 (71%) |
| Office posters | 21 (57%) | 93 (56%) |
| Brief motivational interview training | 20 (54%) | 86 (52%) |
| Communication skill-building (e.g., role-playing) | 18 (49%) | 79 (48%) |
| Waiting room video | 17 (46%) | 95 (57%) |
What's getting in the way?
The authors identified some limitations of their study results:
- Some of the information was collected at a regional conference and that could limit its generalizability.
- All the information was collected at professional conferences, and practitioners who attend conferences could have different attributes from those who don't.
- The results were based on a convenience sample of those who volunteered for focus groups or attended CE sessions where survey data were collected.
- The sample size of those who completed the survey was small and its paper-and-pencil methodology allowed participants to skip questions or provide incomplete data.
However, the authors recommended that dental practitioners continue to screen for HPV-related cancers and become increasingly familiar with ways to prevent HPV-related diseases.
"Although the HPV vaccine has not yet been approved for the prevention of oropharyngeal cancer, dental providers may well become the next line of prevention of this rapidly increasing oral health concern," they concluded.



















