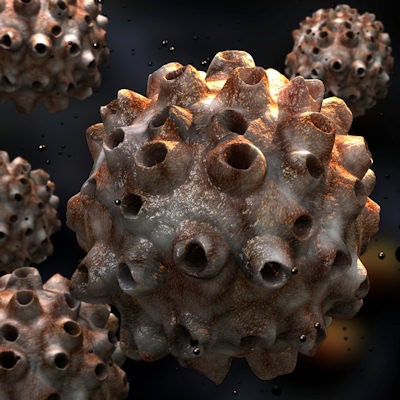
Can dentists and hygienists help prevent oropharyngeal cancers? The authors of a new study suggest being informed about the human papillomavirus (HPV) and the ability to talk with patients about this difficult topic may help reduce the incidence of these cancers.
Wanting to learn more about dentists' knowledge about HPV and their willingness to talk with their patients about the issue, researchers from the University of South Florida conducted focus groups with a total of 33 dentists participating. They found that most dentists do not discuss HPV prevention strategies with their patients for a variety of reasons.
"Given the alarming increase of HPV-attributable oropharyngeal cancers, dentists and dental hygienists may be key agents for promoting HPV prevention," noted lead investigator Ellen Daley, PhD, a professor at the university's College of Public Health, in a statement. "However, there's a serious need for better training and education in the dental community."
The study was published in the Journal of the American Dental Association (January 2018, Vol. 149:1, pp. 9-17).
A little more conversation
Oropharyngeal cancers affect the base of the tongue, the tonsils, and the walls of the pharynx. Three-quarters of these cancers are caused by HPV, according to the study authors.
“Given the alarming increase of HPV-attributable oropharyngeal cancers, dentists and dental hygienists may be key agents for promoting HPV prevention.”
In the U.S., the HPV vaccination program is provider-based, meaning that the vaccine's use depends on a provider's recommendation. While the study authors acknowledged that many factors play a role in whether someone receives the HPV vaccine series, a provider's recommendation plays a significant role in shaping patients' intention to receive it.
The researchers wanted to find out what dentists know about HPV and its connection with oropharyngeal cancer. To do so, they conducted four focus groups at a regional dental conference in 2016, with a total of 33 dentists participating.
Of the 33 dentists, 19 were male and 21 identified as general or family dentists. The average age of participants was just under 47.
The participating dentists were asked several questions:
- What do they know about HPV, and where do they get their information?
- Did they know there is a vaccination for HPV?
- How do they apply their information about HPV?
- Did they, or their hygienists, screen patients for oral cancer?
Participants responded that they received their information from various sources, including dental journals, continuing education courses, and their colleagues. They also mentioned receiving information from the ADA, popular magazines and TV shows, and friends and family, and they also stated when they attended dental school.
Most participants understood that HPV was a sexually transmitted infection that could cause cancer, the researchers reported. The dentists also knew that a vaccine for preventing its infection existed.
But when it came to their working knowledge of the vaccination process, some participants responded that they thought the vaccination had been removed from the market because of vaccine-related health risks and birth defects, or they believed that it provided protection only against low-risk HPV. The researchers noted that this information was incorrect.
"In general, participants knew that both male and female adolescents should receive the HPV vaccine," the authors wrote. "However, participants asked the focus group moderator many questions regarding specific vaccine age and sex recommendations, as well as insurance coverage for vaccination, illustrating an interest in obtaining more HPV-related information."
On the subject of patient oral cancer screenings, most dentists in the focus groups indicated that they or their hygienists regularly performed these screenings. Not all participants, however, informed their patients that they were completing a screening.
"Why would we talk about that if we see no signs and symptoms of it?" the researchers quoted one dentist as saying.
However, the dentists did say they would discuss HPV-related oropharyngeal cancer information with patients if they saw evidence of an infection.
The practitioners were asked about what could influence whether they would discuss the relationship between HPV and oropharyngeal cancer with their patients. Patient and practice factors were the two themes that came up most frequently. Patient factors included a patient's age, their risk profile, difficulty discussing a sensitive topic with patients, and whether the patient had symptoms consistent with oropharyngeal cancer. Practice factors included the physical layout of the office, as participants noted they had an open operatory layout, which provided insufficient privacy to discuss a sensitive topic.
Most participants were not discussing HPV-related cancer prevention with their patients, the study authors concluded.
Intervention needed
The researchers noted that their focus group discussions indicated areas for intervention:
- Creating awareness of trusted information sources
- Improving HPV knowledge
- Understanding the multiple appraisal factors
- Enhancing communication skills of dentists with patients
Having said that, they also acknowledged their study's limitations, such as a tendency of focus group participants to give opinions they think others want to hear, as well as the fact that participants were attending a regional conference and their knowledge may differ from dentists and hygienists in other regions. In addition, most of the participants worked in a private practice setting; thus, generalization to other types of practices is limited.
They also noted that while larger studies are needed in the future, their findings are relevant to daily practice, despite the study's small size.
"These findings are relevant to clinical practice because they highlight modifiable barriers to the discussion of the prevention of HPV-related oropharyngeal cancers between dentists and patients," they wrote.



















