The Georgia Dental Association (GDA) recently launched a campaign, Because I Saw My Dentist, which is part of a larger initiative, the Action for Dental Health. The campaign is meant to address barriers to oral healthcare and improve oral health for Georgians.
Yet the association adamantly opposed HB 684, a bill introduced by the Georgia Dental Hygienists' Association, that not only broke down barriers to oral healthcare but increased access to preventive and therapeutic dental hygiene services for underserved residents.
Conveniently for the GDA, its initiative falls on the heels of the defeat of HB 684, which the association worked to kill.
 Suzanne Newkirk, RDH, is a dental hygiene coach and mentor.
Suzanne Newkirk, RDH, is a dental hygiene coach and mentor.A large body of published research literature on preventive dental visits and services demonstrates that this proactive care is effective in reducing disease and improving oral health for both children and adults. Additionally, preventive care may alleviate pain before it begins, help avoid costly invasive oral procedures, improve quality of life, and save lives through the early diagnosis of life-threatening conditions such as oral cancer. Preventive care has also proved to be cost-effective.
Without access to regular preventive dental services, dental care for many is postponed until symptoms, such as toothache and facial abscess, become so acute that care is sought in hospital emergency departments. This frequent consequence of failed prevention is not only costly to Georgians, but it rarely addresses the problem, as few emergency departments deliver definitive dental services. As a result, patients typically receive only temporary relief of pain through medication and, in some acute cases, highly costly surgical care.
HB 684 required no funding and would have fostered the potential to reduce the $47 million annual cost to Medicaid, Medicare, and other payors for dental emergencies seen in hospital emergency departments around the state.
Barriers to care
An aspiration of the Because I Saw My Dentist campaign is for patients to find a dental home. Yet the GDA disregarded the fact that patients seen by dental hygienists working in the safety-net facilities under HB 684 would have had the opportunity to establish a dental home with the supervising (private practice) dentist or in one of the safety-net facilities listed in the bill, such as private Medicaid practices, nonprofit health centers, or a federally qualified health center.
In his column, "Dispelling myths about barriers to care and Ga. House Bill 684,", GDA Executive Director Frank Capaldo stated that the bill did not address barriers to care, such as language, cost, fear, time off from work, or securing parental permission in school settings. Yet nowhere in its Georgia Action for Dental Health initiative does the GDA provide solutions that address these same barriers.
Sadly, GDA's campaign is nothing more than bombastic rhetoric that completely misses the mark as it pertains to the real issues affecting Georgians. As we've noted, statistics show that nearly 1 in 5 Georgians lives in poverty, and a third of the population is African-American, many of whom are economically disadvantaged, comprising 45% of the state's impoverished residents. In the state, 12% of residents are age 65 years or older, and 25% of the population are children 18 years or younger.
Untreated dental decay is the leading chronic disease of childhood. Untreated tooth decay among low-income children in Georgia is 50% higher than tooth decay among Georgia children of a higher socioeconomic status. In the state, 1 in every 4 children lives in a low-income household, and only 50% of Georgia Medicaid-eligible children receive preventive dental services.
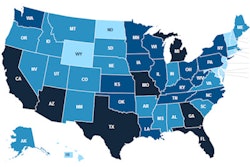
The Georgia State Office of Rural Health classifies 108 counties in Georgia as rural and 51 as nonrural. Almost 90% of Georgia's rural counties are considered dental health professional shortage areas, 43% of the nonrural counties are in the same boat, and 16 counties in Georgia having no dentist at all. HB 684 would have broken down barriers and expanded services for these population groups.
Capaldo stated that the residents living in the 16 counties without a dentist are within a 30-minute drive to the closest dentist in a neighboring county. However, he failed to mention how many of these neighboring dentists are willing to see these patients at no charge or at reduced fees. Further, the GDA provides no evidence as to how these private dental practices are any more equipped to address language barriers, fear, and time off from work than the expanded safety-net settings listed under HB 684.
GDA's initiative lacks a critical piece -- enhancing the dental workforce. Almost every report and study released since the first U.S. surgeon general's Oral Health in America report includes this important aspect for breaking down barriers and increasing access to care.
“Is it any wonder Georgia lags behind the rest of the country with regard to oral health access and prevention?”
A 2011 Institute of Medicine and National Research Council report, titled Improving Access to Oral Health Care for Vulnerable and Underserved Populations, recommended that state legislatures amend existing state laws, including practice acts, to maximize access to oral healthcare to allow allied dental professionals to practice to the full extent of their education and training. The report also stated that allied dental professionals be allowed to work in a variety of settings under evidence-supported supervision levels and allow technology-supported remote collaboration and supervision.
HB 684 encompassed all these recommendations, yet the GDA steadfastly opposed the bill, stating it posed a public safety issue. Which makes one question how the GDA could possibly know more about safety for allied dental professionals than the Institute of Medicine and the National Research Council?
A 2014 National Governors Association report summarized what many states already know -- that expanding the oral healthcare workforce, especially dental hygienists, will decrease barriers to access, particularly in underserved and vulnerable populations. The report identified that to increase access to effective interventions that show cost savings, states should consider expanding scope-of-practice laws and change Medicaid reimbursement policies to expand opportunities for all dental professionals, including dental hygienists to practice to the full extent of their licenses.
It is unfortunate that with all the information available in numerous published studies by experts in its field, the best GDA is able to come up with to improve the oral health of Georgians is a campaign titled Because I Saw My Dentist.
Is it any wonder Georgia lags behind the rest of the country with regard to oral health access and prevention?
Suzanne Newkirk, RDH, is a dental hygiene coach and mentor and a recognized key opinion leader in dental endoscopy. Her website is www.perioscopyprofessionals.com, and she can be reached at [email protected].
The comments and observations expressed herein do not necessarily reflect the opinions of DrBicuspid.com, nor should they be construed as an endorsement or admonishment of any particular idea, vendor, or organization.