Transoral robotic surgery (TORS) alone could provide better quality of life and outcomes for patients with oropharyngeal squamous cell carcinoma (OPSCC) than treatment with adjuvant radiotherapy or chemoradiotherapy, according to a study in JAMA Otolaryngology -- Head & Neck Surgery (April 2, 2015).
In 2009, the U.S. Food and Drug Administration (FDA) approved the da Vinci robotic surgical system (Intuitive Surgical) for use in TORS, a minimally invasive procedure in which the system translates the surgeon's hand motions into small movements of surgical instruments.
"Surgery alone is an effective option for patients with low-volume oropharyngeal cancer," senior author Umamaheswar Duvvuri, MD, PhD, assistant professor of otolaryngology at University of Pittsburgh Medical Center (UPMC), told DrBicuspid.com. "Importantly, in selected patients, we can avoid chemotherapy or radiation completely. In these patients, the functional outcomes of surgery are excellent."
Shifts in treatment
There have been significant shifts in the recommended treatment of patients with oropharyngeal squamous cell carcinoma because of technological advances in all treatment modalities in the past 30 years. The use of primary chemoradiotherapy for OPSCC has doubled, while the use of primary radiotherapy and primary surgical therapy has decreased.
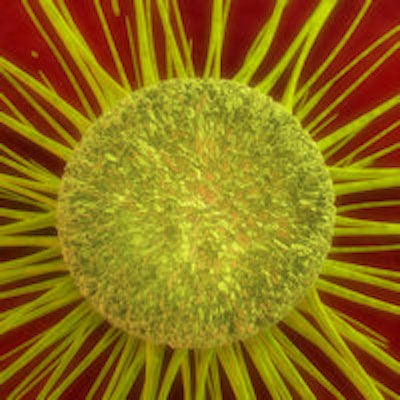
 Umamaheswar Duvvuri, MD, PhD, with the TORS system. Image courtesy of UPMC.
Umamaheswar Duvvuri, MD, PhD, with the TORS system. Image courtesy of UPMC.However, acute and late toxic effects are a limiting factor for successful treatment with radiation therapy and chemoradiotherapy. Common adverse effects include mucositis, xerostomia, dysgeusia, and an increased risk of oral infections, all of which impair post-treatment quality of life.
"The present study is especially timely in the current era of human papillomavirus-positive OPSCC, with younger and healthier patients seeking treatment modalities with less long-term treatment-related morbidity," the authors noted.
Over the past decade, the use of TORS as a treatment option for OPSCC has been increasing. Multiple studies have shown that TORS, with or without adjuvant therapy, offers excellent long-term oncologic and survival outcomes. It has also been associated with decreased hospitalization and less need to place tracheostomy or gastrostomy tubes.
TORS can be used to safely and efficiently remove tumors previously thought to be inoperable. It can also be used in cases that necessitate highly invasive surgical techniques in combination with chemotherapy or radiation therapy.
Current surgical techniques to reach the deepest areas of the head and neck can require external incisions to the patient's neck or splitting of the jawbone or areas close to the voice box.
With TORS, the surgeon, working from an operating console close to the patient, operates miniature robotic "arms" that can navigate through the small and delicate areas of the mouth without the need for external incisions. A retraction system allows the surgeon to see the entire surgical area at once.
Retrospective review
In the current study, a retrospective review, the researchers analyzed the use of TORS alone for patients with early-stage OPSCC and described quality-of-life outcomes up to two years after treatment.
The researchers evaluated the medical records of 34 patients (mean age, 59 years) at University of Pittsburgh Medical Center who had TORS as the primary treatment for OPSCC between May 2010 and March 2014.
“Surgery alone is an effective option for patients with low-volume oropharyngeal cancer. Importantly, in selected patients, we can avoid chemotherapy or radiation completely.”
Ninety-four percent of the patients were white and 76% were men. Most patients had T1 (59%) or T2 (38%) and N0 (38%) or N1 (47%) disease. The most common oropharyngeal primary subsite of cancer was the tonsil (47%), followed by the base of tongue (44%).
Patients who received postoperative chemoradiotherapy or radiotherapy were excluded from the study.
The subjects completed a questionnaire before surgery and at one-month, six-month, one-year, and two-year postoperative checkups. They were asked to rate their quality of life on a scale of 1 to 100, with 100 representing the best score. The median follow-up was 14 months.
General quality of life -- including pain, swallowing, activity, and chewing -- showed consistent improvement during follow-up. A significant improvement in chewing scores occurred in the first one to 12 months after surgery (p = 0.048) and a positive chewing score was found over time (p = 0.05).
Significant pain improvements occurred at one to six months (p = 0.006) and one year (p = 0.01) after surgery; however, this score did not continue to improve over time. Swallowing scores showed improvement from one to six months (p = 0.047) and at two years (p = 0.048) after surgery. The median activity score also improved over time (p = 0.03).
"We didn't expect to see such a big effect," Dr. Duvvuri said, noting that patients were almost back to baseline condition by 24 months. "This suggests that surgery alone is a great way for patients to get back to their regular activities as quickly as possible. Existing data suggests that many patients never get back to baseline after chemoradiation. Therefore, surgery may be a better option for certain select patients."
Two patients (6%) died during follow-up, one due to disease progression and the other due to myocardial infarction. Two patients required temporary gastronomy tube placement, and none of the patients required a tracheostomy.
The researchers cited the small cohort size and the fact that not all patients completed survey forms as limitations of the study.



















