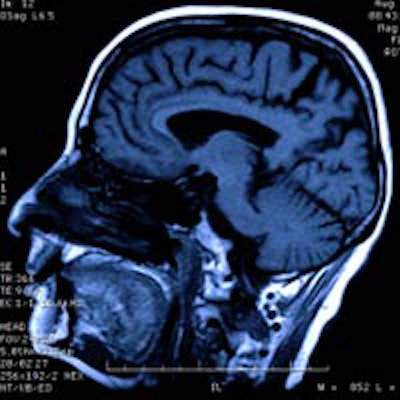
Magnetic resonance imaging (MRI) may be a better tool for predicting the chances of survival and tumor metastasis of patients with oral cancer, according to a new study by British researchers. They found that measuring tumor volume on MRI scans could offer a more accurate prognosis than analyzing the surface area of a tumor.
MRI demonstrated promising results in a dual-center, retrospective study by researchers at University of Oxford's Radiology Group at John Radcliffe Hospital and the University College London Eastman Dental Institute Department of Oral & Maxillofacial Surgery and published in the British Journal of Oral and Maxillofacial Surgery (September 27, 2013).
"We have shown that tumor volume and thickness measured on MRI is significantly related to two-year disease-related survival and occult cervical lymph node metastasis," the researchers wrote. "Measurements of volume and thickness on MRI have the potential to provide valuable information that will guide preoperative decisions."
Drawbacks of TNM system
The tumor, node, and metastasis (TNM) staging system is commonly used by clinicians to predict patient prognosis for a wide variety of cancers. For oral cancer, this system is based on surface diameter of a tumor; this works well for large, superficial tumors but is less suitable for small, deep cancers. Better identification of oral cancer patients could prevent unnecessary elective neck dissection where there are no signs of regional metastases.
Previous studies have established that MRI can properly evaluate thickness, or the distance from the surface to the deepest point of the tumor's invasion, the researchers explained. And their own work found that tumor volume measured on MRI can predict occult cervical lymph node metastasis and survival in lingual carcinoma using cut-points of 3 cm3 and 8 cm3, respectively.
The researchers had two goals: "First, we aimed to investigate whether tumor volume and thickness could be used to predict 20-year disease-related survival, and whether it could be used in a refined TNM staging system," they wrote. "Secondly, we aimed to use these data to predict occult cervical lymph node metastasis and to propose a new decision rule for elective neck dissection."
The researchers sourced their study population from patients with confirmed squamous cell carcinoma (SCC) of the oral cavity who were treated at John Radcliffe Hospital from 1998 to 2008 and Oxford and University College London Hospital from 2006 to 2008. The study considered 397 consecutive patients, and 199 were included after exclusions were applied for reasons such as inadequate or unrecoverable MRI studies and records or SCC of the lip, since they are rarely imaged.
Next, they measured tumor volume with manual segmentation and thickness measured from the tumor's surface to the deepest point of invasion. In cases without a visible histologically confirmed occult cervical metastasis, the researchers assigned a volume and thickness of 0 cm3 and 0 mm.
Among the 199 study subjects, 29 disease-related deaths occurred.
In their data analysis, the researchers observed a strong correlation between tumor thickness measured on MRI and the depth of tumors on histology. The median depth on MRI was 11.2 mm (range of 4.4-16.4 mm), compared with a median histological depth of 10.0 mm (range of 4.8-15.0 mm). The correlation coefficient, demonstrating the relationship between the two variables, was r = 0.79 (p < 0.001).
They also noted that tumor volume grouped with the 3 cm3 cut-point served as a significant predictor of disease-related survival, which was defined as a death that occurred within the two-year follow-up period due to disease and not surgical complications. Cut-points of 0.5 cm3 and 8 cm3 also were significant.
"Grouping the cases into quartiles provides low-, intermediate-, and high-risk groups with respective two-year mortalities of 2%, 15%, and 31%," the researchers wrote. "For thickness quartiles of 4.0 mm and 16.0 mm, there was a similar stratification with mortalities of 0%, 14%, and 29%."
The similar pattern developed in predicting occult cervical lymph node metastasis, as the researchers observed that grouping tumor volume into 0.5 cm3 and 8 cm3 quartiles yielded low-, intermediate-, and high-risk groups.
"Tumors with a volume or thickness that was less than the first quartile had a 4.3% and 5% chance of metastasis, respectively," the researchers explained. "These patients may be spared elective neck dissection."
"Tumor volume and thickness, when grouped using quartiles 0.5 and 8 cm3, and 4.0 and 16 cm3, may indicate low-, intermediate-, and high-risk groups for survival and predict occult cervical lymph node metastasis," the researchers concluded.
T classification did not identify the risk as accurately, as it is similar among T1, T2, and T3 tumors. Indeed, the researchers described measuring volume and thickness as "superior to the current TNM staging system."