The mouth provides a hospitable environment for many microorganisms. It is warm, nutrient-rich, continuously bathed with saliva, and has a pH of between 6.75 and 7.25. Hence the oral cavity is home to a rich microbiota, most of which are beneficial organisms and live in harmony with each other and the host.
The presence of microbes is in fact essential for maintaining the normal physiology of the oral cavity. While this symbiosis is usually stable and mutually beneficial, if some external force changes the balance, the result can be gingivitis, dental caries, or periodontal disease.
A significant body of knowledge is now available on how to maintain a healthy ecology of microbiota and keep diseases at bay. There is also a growing number of oral health products, from lozenges to mouthwashes, designed to optimize the balance of bacteria in the mouth, retain their beneficial characteristics, and suppress their potentially harmful impact.
Denizens of the oral cavity
Philip D. Marsh, PhD, is one of the leaders in this area and has been publishing papers on oral microbes for more than 35 years. He advises caution when seeking to interfere with the microbiological balance in the mouth in a bid to stem oral diseases.
"What we've been brought up with is 'Plaque is bad -- get rid of it.' But it's actually too much plaque and plaque in the wrong places that are bad for us. We want to prevent the buildup of levels of organisms, particularly in hard-to-reach places of the mouth, that could lead to disease," said Marsh, a professor of oral microbiology at Leeds Dental Institute. "Pushing to have an ultraclean mouth isn't beneficial to us; we should be trying to maintain our natural microbiota at levels compatible with oral health in order to preserve their beneficial activities."
Aaron Weinberg, DMD, PhD, agrees that trying to sterilize the mouth may lead the way for exogenous, deleterious organisms to colonize it instead.
"You don't want a sterile mouth; you want a mouth that has primarily good bacteria in it, in order to keep exogenous microorganisms out and prevent them from colonizing the mouth," said Dr. Weinberg, the associate dean for research at the Case Western Reserve University School of Dental Medicine.
Another faculty member at the Case Western Reserve University dental school who specializes in oral bacteria has a similar view. Yiping Weng Han, PhD, a professor of periodontics, pathology, and reproductive biology, focuses on Fusobacterium nucleatum, as does Dr. Weinberg.
According to Dr. Han, the ultimate research goal is not to "search out and destroy" all cells of F. nucleatum, although the microbe is associated with serious diseases in the oral cavity and throughout the body.
"First of all, to eliminate all the bacteria is impractical, and it's also not ideal because then you have a surface that exogenous bacteria can colonize," she said. "Also, if we eliminate one species, we don't yet know the effects because there is a lot of interdependence among different species."
The importance of homeostasis
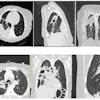
Biofilms form in a rapid sequence of events and mature into a complex, interacting community of microorganisms that have different properties than when they are present in isolation. The resulting community is more resistant to antimicrobial agents, stress, and host defenses, for example. Biofilms act as a barrier to organisms in the air, water, and food with which people constantly come into contact.
Among the main bacteria residing in the mouth -- including in biofilms -- in both health and disease are species that have traditionally been considered to be "bad," such as Streptococcus mutans, Tannerella forsythia, Porphyromonas gingivalis, and F. nucleatum. The bacteria that have been picked for the "good" team include S. sanguinis, S. oralis, Actinomyces naeslundii, Neisseria subflava, and Veillonella dispar.
However, it is now acknowledged that this is an artificial distinction. For example, F. nucleatum has been shown by the teams led by Drs. Weinberg and Han to have properties that can be exploited to benefit human health. But F. nucleatum is also associated with gingivitis and a raft of serious diseases elsewhere in the body.
"While it is debatable whether F. nucleatum is a 'good' or 'bad' bug in the oral cavity, as soon as this fastidious anaerobe leaves its natural habitat -- that is, the mouth -- it becomes a bona fide 'bad' bug," Dr. Han noted.
Several decades ago, researchers likened the interactions in the mouth to ecological systems in nature. Breakdowns in the normal balance between species on the planet can result from a number of causes and hence do not have one exclusive etiology. Similarly, Dr. Marsh believes, in the mouth, the key steps in the descent into disease relate to particular shifts in environmental circumstances rather than the actions of specific sets of microorganisms.
"If you take 100 examples of an organism that is implicated in dental caries -- S. mutans, for example -- you can find some that are very good at making acid and some that are not quite as good," Dr. Marsh explained. "We're not dealing with bacteria that produce toxins. We're dealing with bacteria whose metabolic end products can be deleterious and which grow best in the presence of those end products."
Dr. Weinberg has a similar view.
"This concept of 'pathogenic organisms' is really overutilized," he said. "Because when you say 'pathogenic organism,' you're equating it to something that shouldn't be in the body. But in oral disease, these are organisms that have evolved over the millennia to grow and coexist with the host, albeit in low numbers."
Dr. Weinberg's own research with F. nucleatum indicates that when the bacterium comes into contact with oral epithelial cells, the cells produce small proteins, which he has dubbed human beta-defensins. These are a group of antimicrobial peptides that kill bacteria, fungi, and encapsulated viruses, and represent the first line of defense for the mouth's lining. Dr. Weinberg's team has also isolated and characterized, from the outer membrane of F. nucleatum, the F. nucleatum-associated defensin inducer (FAD-I), which promotes the expression of human beta-defensins (Journal of Biological Chemistry, November 19, 2010, Vol. 285:47, pp. 36523-36531).
The team now is working to identify the "hot spots" of FAD-I that are directly responsible for this activity. The goal is eventually to be able to control and direct the production of endogenous antimicrobial peptides in the oral mucosa and other vulnerable mucosal sites of the body.
"The idea is to use FAD-I in certain situations in the oral cavity where you want a particular site to be more sterile than others," Dr. Weinberg explained. "If you can induce the production of these peptides -- which are nature's own antibiotics -- we could possibly change the microflora of that particular site. And if we could use the peptides as an adjunct to conventional antibiotics, we may be able to reduce the antibiotic resistance that is prevalent in a number of bacteria."
For their part, Dr. Han and her co-investigators have begun identifying the mechanisms that allow F. nucleatum to move from the mouth into the bloodstream and thence throughout the body -- taking other bacteria with it and leaving destruction in their path (Molecular Microbiology, December 2011, Vol. 82:6, pp. 1468-1480). Her team has shown that F. nucleatum can induce preterm birth and stillbirth in animals and humans (see, for example, Obstetrics & Gynecology, February 2010, Vol. 115:suppl 2, part 2, pp. 442-445). Other researchers have linked it to colorectal cancer (Genome Research, October 18, 2011) and infections and abscesses in all the internal organs, including the brain and lungs.
A fine balance -- that can be destroyed
In a healthy mouth, biofilms perform many positive functions. As just one example, 25% of nitrates from vegetables re-emerge in the saliva. In the mouth, the nitrates are converted to nitrites, which in turn are converted to nitric oxide in the stomach (Free Radical Biology & Medicine, April 2009, Vol. 46:8, pp. 1068-1075). Nitric oxide has many important functions in maintaining good health, including helping control blood pressure.
In addition, some beneficial bacteria are now recognized as being capable of signaling to their hosts -- us -- that they are not harmful.
"It has been shown -- first in the gut and now there are a couple of papers in dental journals on this relating to oral bacteria -- that the bacteria 'talk' to the host to indicate they are beneficial: 'Don't overreact to us, because we're doing you good.' That allows the host to focus, instead, on searching for microorganisms that are actually potential threats," said Dr. Marsh, citing one of several papers on the topic (Infection and Immunity, September 2008, Vol. 76:9, pp. 4163-4175).
When the natural balance in the mouth shifts significantly, bacteria with harmful effects can begin to dominate. pH and nutrient status are believed to be two of the main drivers of the descent into disease. For example, in people who have a diet high in simple carbohydrates or sugars, the pH of the mouth will drop more frequently and to lower levels than in people with a more healthful diet. This in turn leads to a significant increase in acid-tolerating bacteria such as S. mutans and the displacement of oral-health-associated, neutral-pH-loving bacteria.
Another example is the increase in gram-negative proteolytic bacteria in the presence of the inflammatory response that accompanies periodontal disease. These proteolytic bacteria can further exacerbate the inflammatory response, leading in turn to even worse damage to the teeth and surrounding tissues, as well as greater proliferation of damaging bacteria.
"So it's a change in environment that selects for the more pathogenic organisms," Dr. Marsh explained. "Therefore, to deal with disease, it's not the best approach to only try to develop an agent that is 'antiorganism X' or 'antiorganism Y,' but rather to also try to deal with the pressures that cause the selection. Otherwise, it'll just happen over and over again."
Other researchers have uncovered some interesting potential twists in this view of the oral microorganism-disease interaction. George Hajishengallis, DDS, PhD -- who recently moved from the University of Louisville to the University of Pennsylvania -- and his colleagues are challenging the traditional view of P. gingivalis' role in periodontitis (Cell Host & Microbe, November 2011, Vol. 10:5, pp. 497-506).
They hypothesize that P. gingivalis acts as a "keystone pathogen" and co-opts other bacteria into the destruction of bone. The scientists have shown that P. gingivalis is able to induce an inflammatory response to its presence without itself being attacked by inflammatory cells. The result is a flood of exudate into the periodontal space, which feeds both P. gingivalis and other bacterial species in the biofilm. The well-fed miniature army then proceeds to induce even more inflammation, which destroys the bone and surrounding tissue.
"So it's actually the altered microbiota that are causing the bone loss, not P. gingivalis itself, which remains at low concentrations," Dr. Hajishengallis said.
The key to this process is the ability of P. gingivalis to subvert the function of a key receptor on the surface of some inflammatory cells that recognizes a molecule known as complement component 5. Complement component 5 plays a crucial role in the inflammatory cascade. The result is the inflammatory cells are incapacitated. The researchers hope that the use of an antagonist that blocks the receptor can stop this action on the part of P. gingivalis.
"This is promising, and we are testing the possibility in animals," Dr. Hajishengallis said. "If we get encouraging results, we will start on human studies."
Dr. Hajishengallis' excitement at gaining new insights into the ancient relationship between humans and our tiny fellow travelers is shared by every researcher in the field -- including those who use the expanding knowledge to design products that optimize oral health.
New research yields new products
It isn't possible to fully summarize in a few words the wide array of products that is springing from rapidly advancing research. A sampling will provide at least an inkling of the breadth and power of what is available.
One of the major categories of offerings is probiotics. Some companies, such as Nutri-Health Supplements and Life Extension, sell mints that pack a probiotic punch. Life Extension's Advanced Oral Hygiene vegetarian mint lozenges contain both Bacillus coagulans and S. salivarius. The company's website cites studies indicating that in vitro S. salivarius inhibits biofilm formation by S. mutans. Regular use of the lozenges "could make a significant impact in protecting oral health," due to the beneficial bacteria's ability to "help block harmful bacteria ... in the mouth," according to the company.
Toothpaste is another popular probiotic delivery vehicle. Designs for Health's PerioBiotic toothpaste, for example, contains the Lactobacillus paracasei strain ADP-1 -- dubbed Dental-Lac -- as well as xylitol and calcium glycerophosphate.
Mouthwashes that contain antibacterial agents and/or probiotics also have been developed. For example, a team led by Wenyuan Shi, PhD, the chair of oral biology at the University of California, Los Angeles, School of Dentistry and founder of C3-Jian, has produced a mouthwash that contains a specifically targeted antimicrobial peptide (STAMP) called C16G2. Like other STAMPs, C16G2 is designed to selectively kill S. mutans while leaving the rest of the microbiota intact, according to information on C3-Jian's website (the company has exclusive patent rights to the mouthwash). A phase I trial with 12 healthy adult volunteers showed the mouthwash lowered concentrations of S. mutans, and also reduced the plaque burden and amount of demineralization (Caries Research, November 2011, Vol. 45:5, pp. 415-428).
"I like to explain it in terms of the ecology of a lawn," Shi said. "When you use a broad-spectrum herbicide, all of the plants in the lawn get knocked down for a little while, but they also grow back first. It's better to specifically kill the weeds, or bad bacteria."
The ProBiora3 mouthwash from Oragenics contains a mix of three probiotic bacterial strains: S. oralis KJ3, S. rattus JH145, and S. uberis KJ2. The results of a phase I clinical trial involving 20 healthy 21- to 35-year-old volunteers suggested the product is well-tolerated and produced large but not statistically significant drops in S. mutans titers and significant decreases in concentrations of Campylobacter rectus and P. gingivalis (Journal of Applied Microbiology, August 2009, Vol. 107:2, pp. 682-690).
"The science behind the product is fairly definitive, I would say," said Oragenics' co-founder Jeffrey Hillman, DDS, who recently retired as the company's chief scientific officer and director. "And it's been well-received by everyone who's used it. The strains in the mouthwash not only outcompete the 'bad' bacteria, they also produce small amounts of hydrogen peroxide that gradually whiten teeth. So there are cosmetic benefits as well as the benefits to oral health."
When it comes to finding balance in the oral cavity, it's a good time to be a dentist and a patient, it seems. The new avenues of research opening up with every passing day are making the match more even between human ingenuity and bacteria's ancient craftiness.