The National Institutes of Health has given $2.25 million to Case Western Reserve University School of Dental Medicine researchers to study how an isolated agent from common oral bacteria may hold the answer to how human beta defensins could be used to help block bacteria from entering epithelial tissue.
Aaron Weinberg, DMD, PhD, a professor and the chair of the department of biological sciences at the dental school, will lead the research group. The new grant will continue the exploration of their discovery last year of an agent called Fusobacterium nucleatum-associated Beta-Defensin Inducer (FAD-I).
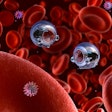
This agent triggers the expression and release of the HBD peptides from epithelial cells that make up the mucosal linings of the body, such as skin, the respiratory track, and the gastrointestinal and urogenital tracks.
The new grant will continue the group's research, with a goal of isolating which strains of F. nucleatum bacteria have more potent FAD-I activity and why, understanding more about the biology and structure of FAD-I, and using a mouse model to see how effective it is as a potential treatment.
The researchers are particularly interested in why FAD-I sets defensins to work without triggering inflammation, which can be a health risk if the inflammation is not abated by the normal defense system. In the mouth, it can cause periodontal disease and eventual tooth loss.
"It started with our observation that when the bacterium comes in contact with human epithelial cells, it promotes the induction of these HBD peptides," Dr. Weinberg stated in a news release.
HBDs put up a defense when challenged by oral bacteria and block the invasion of the more than 700 species of bacteria in the mouth from entering the body.
The researchers have studied the link between the mouth's bacteria and the induction of HBDs for more than a decade, and have unraveled the relationship between this common oral bacterium and the peptides.
In the process of understanding HBDs and oral bacteria by focusing on F. nucleatum, they discovered FAD-I on the surface of the outer membrane of this bacterium. Even when the outer membrane portion containing FAD-I was separated from the main bacterium, FAD-I continued to induce HBD action in vitro. In addition, when researchers genetically expressed FAD-I in other bacteria that didn't induce HBD expression and release from epithelial cells, the bacteria were then able to induce HBD expression and release, Dr. Weinberg explained.
The idea is to promote nature's own antibiotics in sites where they would come in contact with FAD-I, Dr. Weinberg said.
"The possibility exists that FAD-I can induce defensins in other parts of the body where they are found," he explained. "Wouldn't it be neat if we could promote the expression of Mother Nature's own antibiotics in vulnerable sites by intentionally challenging the sites with FAD-I and thereby protecting the sites from microbial challenges?"