
A dental team in Afghanistan identified a dorsal tongue ulcer in a 62-year-old man who later tested positive for COVID-19. The man's painful lesion persisted for weeks, and he also experienced asymptomatic geographic tongue, according to details published on May 20 in BMC Oral Health.
Patients with problems in the oral mucosa and suspected or confirmed SARS-CoV-2 infection should be monitored, noted the authors, led by Dr. Mohammad Bashir Nejabi from Kabul University of Medical Sciences. The team also advised screening patients with COVID-19 for symptoms and findings in the oral cavity.
"To prevent such an outcome, awareness programs need to be implemented for the diagnosis and management of clinical symptoms among patients," the authors wrote.
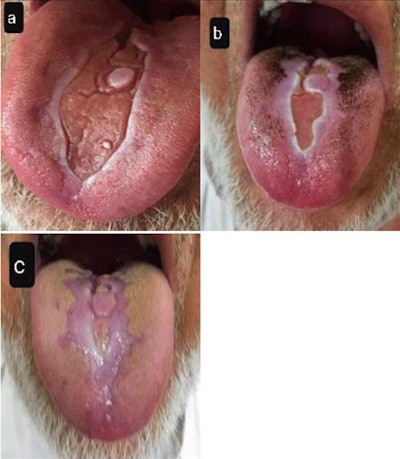 (A) Fissured tongue with white scars immediately after COVID-19 recovery. (B, C) Tongue appearance four weeks after first examination. Image courtesy of BMC Oral Health and Nejabi et al. Licensed under CC by 4.0.
(A) Fissured tongue with white scars immediately after COVID-19 recovery. (B, C) Tongue appearance four weeks after first examination. Image courtesy of BMC Oral Health and Nejabi et al. Licensed under CC by 4.0.The 62-year-old man visited a university dental clinic in August due to a painful erosive ulcer on the dorsal surface of his tongue. The patient's history included type 2 diabetes and hypertension, but he did not have a history of candidiasis, lichen planus, or other oral diseases.
The man said he had experienced the ulcer for one week. He also complained of fever, cough, chest tightness, and altered taste in the past two weeks.
The dental team referred him to a local hospital for COVID-19 testing and treatment. A nasal swab test came back positive for SARS-CoV-2 infection, and the treating clinicians prescribed the man with daily azithromycin and twice daily ceftriaxone.
Two weeks later, the man no longer tested positive for COVID-19 and he returned to the dental clinic for treatment. All of his symptoms had resolved except for the painful tongue lesion. However, further testing was positive for herpes simplex virus 1 (HSV-1).
The authors noted a white geographic ulcer with irregular borders on the dorsum of the tongue. The dentist treated the man with intravenous acyclovir 5 mg/kg three times a day for one week, but the treatment had no effect on the oral lesion. He also prescribed photobiomodulation therapy for 10 days, which relieved the man's symptoms.
The lesion partially resolved 11 days after photobiomodulation therapy. During a follow-up examination, the man presented with fewer clinical symptoms, and the size and mass of the lesion were downgraded from severe to moderate.
This isn't the first case of changes to the oral mucosa documented in patients with COVID-19 or who have recovered from SARS-CoV-2 infection. Evidence has shown that a variety of oral manifestations, including ulcers, tongue swelling, and geographic tongue, may be linked to infection with SARS-CoV-2.
"The occurrence of oral signs and symptoms should be considered in COVID-19 patients, including dysgeusia, petechiae, candidiasis, traumatic ulcers, HSV-1 infection, geographical tongue, thrush-like ulcers, among others," the authors wrote.



















