What's the best way to determine the type of oral mucosal lesion a patient may have? Can symptoms such as xerostomia and differences in saliva help distinguish oral lichen planus, oral lichenoid lesions, and stomatitis in patients with or without contact allergies? Researchers sought to find out.
They examined whether individuals with oral lichen planus, oral lichenoid lesions, and generalized stomatitis and concomitant contact allergies had differences in certain symptoms, hypothesizing that these patients had more frequent and severe xerostomia and also differences in saliva and salivary flow than those with the conditions without contact allergies and healthy individuals.
The research team found a greater prevalence of xerostomia among patients with oral lichen planus, oral lichenoid lesions, or stomatitis than healthy individuals but no other significant findings.
"Our findings do not aid in the discrimination between oral lichen planus and oral lichenoid lesions and these conditions with or without contact allergic reactions," the study authors wrote (BMC Oral Health, June 29, 2017).
They were led by Kristine Røn Larsen, a research assistant in the department of odontology at the University of Copenhagen Faculty of Health and Medical Sciences in Denmark.
Staying dry
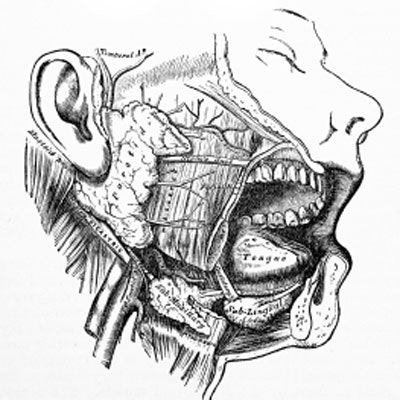
Healthcare practitioners can have a hard time distinguishing between oral lichen planus and lichenoid lesion. The former is one of the most common oral mucosal lesions, affecting 0.5% to 2% of adults, primarily middle-aged and elderly people, and more women than men. Believed to occur due to a T-cell-mediated response of unknown etiology, oral lichen planus may present as reticular, erythematous, ulcerative, plaque-like, bullous, and papular lesions mainly occurring on the buccal mucosa, gingiva, and tongue, the authors explained.
Clinical and histopathological criteria are used to diagnose lichen planus. However, lichenoid lesions are clinically and histopathologically similar, and they can occur because of a reaction to systemic medications or dental materials, as well as contact sensitivity to substances, such as flavorings contained in oral hygiene products.
Xerostomia is often caused by salivary gland hypofunction but can occur with normal-appearing salivary function, and it has been associated with lichen planus and lichenoid lesions. Both can occur with conditions associated with xerostomia and salivary gland hypofunction, such as Sjögren's syndrome, the authors noted. It remains unclear whether xerostomia and other sicca symptoms are due to the two conditions on their own or an association with systemic autoimmune diseases in which xerostomia and salivary gland dysfunction are common.
In addition, immunoglobulin G (IgG) and secretory immunoglobin A (sIgA) are major classes of antibodies contained in human saliva that may play a role in lichen planus pathogenesis. These antibodies could prove useful for distinguishing the condition from lichenoid lesions, according to the authors.
The researchers conducted their study to investigate whether the following factors could be used as diagnostic tools to distinguish between patients with oral lichen planus, lichenoid lesions, and generalized stomatitis with and without concomitant contact allergies, as well as between patients with these conditions with contact allergies and healthy controls:
- Xerostomia frequency
- Xerostomia severity
- Unstimulated and chewing-stimulated whole saliva and citric-acid-stimulated parotid saliva flow rates
- Salivary concentration of total protein and sIgA
The study included 52 Caucasian patients from the oral medicine clinic at the University of Copenhagen who were diagnosed with one of the three conditions, and 49 (94.2%) of them completed the study. They all reported oral symptoms that included stinging and burning sensations. Those with lichen planus and lichenoid lesions had various combinations of reticular, erythematous, ulcerative, and plaque-like mucosal changes. Diagnosis was confirmed by biopsy and histopathological examination, although this method still needs to be tested in larger studies, the authors noted.
Patients with lichen planus or lichenoid lesions were pooled into one group, since distinguishing between them was difficult. Stomatitis patients were diagnosed by having more diffuse, widespread oral mucosal erythema.
For the control group, 29 healthy age- and gender-matched subjects were recruited from a Danish website for study subjects. Exclusion criteria were past or current history of systemic or oral diseases and medication use; however, four controls older than age 65 who used antihypertensive medication were included, since recruiting healthy subjects of that age who didn't use medication was difficult, the authors noted.
The following was performed for each patient and control:
- Mucosal biopsy
- Patch testing for contact allergy
- Serum testing for thyroid-stimulating hormone
- Interview, consisting of standardized questions about present and past systemic diseases, including allergies, and also daily medication intake, alcohol consumption, tobacco smoking, and oral hygiene
- Questioning about taste disturbances, oropharyngeal functions, and xerostomia symptoms, severity, and daily variations
- Measurements of unstimulated and paraffin-chewing-stimulated whole saliva flow rates over 15- and five-minute periods, respectively
- Sampling of citric acid-stimulated parotid saliva sampling over a five-minute period
- Total protein concentration (µg/mL) in unstimulated and chewing-stimulated whole saliva determination using a colorimetric assay
- Indirect enzyme immunoassay of whole saliva samples to determine sIgA
Women made up 85% of the study participants, and the average age was 61, with a range of 32 to 77 years. The researchers diagnosed oral lichen planus in 19 patients, of which 15 had the erosive form, and lichenoid lesions in 19 patients. None of the patients had hepatitis C, Sjögren's syndrome, or other autoimmune diseases. The researchers diagnosed the remaining 11 patients with stomatitis.
They found that 19 patients (38.8%) and 10 controls (34.5%) had contact allergies, primarily to perfume mix. Significantly more patients than controls (p = 0.02) had contact allergies to aroma substances in oral hygiene products, particularly in patients with lichen planus and lichenoid lesions (p = 0.01). The most common allergies among patients was to spearmint, and among controls it was to cassia oil.
The researchers found that patients more frequently reported xerostomia (46.9% versus 20.7%) and greater severity of it than controls, as expected. However, they found no differences in xerostomia severity and prevalence between those with lichen planus or lichenoid lesions and those with generalized stomatitis with and without contact allergies. They also found no associations between the presence and severity of xerostomia and age, gender, number of medical conditions or diseases, or the number of medications taken daily.
| Results of questionnaire on xerostomia | ||
| Healthy controls (n = 29) | Patients (n = 49) | |
| No feeling of dry mouth (score 0) | 79.3% | 53.1% |
| Slight feeling of dry mouth (score 1) | 20.7% | 26.5% |
| Severe feeling of dry mouth (score 2) | 0% | 8.2% |
| Annoying feeling of dry mouth making speech difficult (score 3) | 0% | 12.2% |
| Difficulty swallowing due to xerostomia | 0% | 12.2% |
| Difficulty chewing due to xerostomia | 0% | 10.2% |
| Difficulty eating dry food substances due to xerostomia | 0% | 32.7% |
| Taste perception different from normal | 0% | 28.6% |
| Xerostomia at all times of day | 0% | 10.2% |
| Waking up due to xerostomia | 17.2% | 34.7% |
The researchers found no significant differences in salivary flow rates between the patient and control groups, although unstimulated whole salivary flow rates were lower in patients with lichen planus or lichenoid lesions and concomitant contact allergies than in those without contact allergies (p = 0.05). Additionally, salivary flow rates did not differ by age, gender, number of medical conditions or diseases, number of medications taken daily, or xerostomia prevalence or severity.
Total protein concentrations in unstimulated whole saliva were higher in patients than controls, while they were lower in chewing-stimulated whole saliva, but these differences were not significant. Patients with lichenoid lesions with and without concomitant contact allergies did not differ in total salivary protein concentrations. Levels of sIgA were higher in unstimulated and chewing-stimulated whole saliva in patients than controls, but these differences were not significant either. Salivary sIgA levels among patients with the oral conditions with and without concomitant contact allergies did not vary.
| Mean salivary flow rates | |||
| Healthy controls (n = 29) | Patients (n = 49) | p-value | |
| Unstimulated saliva flow rate (mL/min) | 0.39 | 0.33 | 0.33 |
| Paraffin-chewing-stimulated saliva flow rate | 1.75 | 1.69 | 0.25 |
| Citric-acid-stimulated parotid saliva flow rate (mL/min) | 0.15 | 0.15 | 0.56 |
| Unstimulated total protein concentration (µg/min) | 1131.0 | 1047.9 | 0.86 |
| Paraffin-chewing-stimulated total protein concentration (µg/min) | 4090.0 | 4317.6 | 0.58 |
| Unstimuated sIgA (µg/min) | 47.8 | 48.6 | 0.82 |
| Paraffin-chewing-stimulated sIgA (µg/min) | 82.4 | 96.1 | 0.19 |
Can't tell the difference
The authors noted that xerostomia is often associated with salivary gland hypofunction, but they did not find any associations among xerostomia, its severity, and salivary flow rates.
"Thus, it is likely that the inflammatory changes in the oral mucosa due to oral lichen planus, oral lichenoid lesions, and generalized stomatitis lead [to] sensory disturbances, including sensation of oral dryness," they wrote.
They also took note of a March 2016 study published in the Journal of Oral Pathology & Medicine that found that patients with lichen planus presented with worse psychological profiles and sleep disturbances, as well as high sIgA, cortisol, and total protein levels, than controls. They speculated about the connection of these findings to the current study.
"It is likely that the higher prevalence and more severe xerostomia, the higher salivary concentrations of total protein and levels of sIgA that we find may be ascribed to a higher degree of anxiety, depression, and sleep disturbances in the patient group," the authors wrote.
Overall, xerostomia was the main difference found between patients and controls in the study, with other factors studied not significantly different, and the findings not helping to distinguish between lichen planus and lichenoid lesions.
"Xerostomia is prevalent in patients with oral lichen planus, oral lichenoid lesions, and generalized stomatitis, but not associated with salivary gland hypofunction, number of systemic disease or medications, contact allergy, age, or gender," they concluded.