Combining 3D imaging with clinical findings yields indisputable evidence that becomes the foundation for a complete dental examination. Proper diagnosis is the direct result of gathering and reviewing these findings. The question then becomes, "Should I treat this patient or refer to another dentist?"
If I could not administer treatment at the standard of care, then I would not hesitate to refer the patient to a specialist who could.
 Anthony Ramirez, DDS.
Anthony Ramirez, DDS.This article will evaluate how 3D imaging influenced my initial diagnosis and led to my rendering treatment and a scan that led to a specialist referral.
There are many areas where 3D imaging can be instrumental in gaining case acceptance and help support optimal treatment. Seeing the whole picture with Cerec Galileos (Sirona) has elevated the standard of my diagnosis and treatment planning skills. It is impossible to practice at a comparable standard without the use of Galileos. Working smarter and better is directly attributed to the use of 3D imaging. My office is a laboratory of innovation where I evolved into guided implantology. 3D plays a critical role in improving clinical outcomes and ensuring safe predictable diagnostic decisions that always advance the patient experience. I deliver customized and individualized treatment planning to create logical and uneventful implant experiences for each patient I treat.
A hopeless primary canine
The first case illustrates how I have come to treat patients differently by using cutting-edge technologies that facilitate life-changing care. A 27-year-old woman presented for an Invisalign clear-aligner therapy consultation to discuss ways to improve her smile and occlusion. She also wanted options to replace an overretained upper right primary canine.
She had visited other dentists who planned for extraction and removal of her impacted permanent canine before any implant could be attempted. An immediate implant was not possible according to their diagnosis. Knowing our office used Galileos gave her reason to visit us for an enhanced 3D evaluation. Evaluating the scan gave me the necessary information to definitively determine that it was possible to remove the primary canine and replace it immediately without the removal of the impacted tooth.
I think everyone would agree it would be an option to remove the impaction with an invasive oral surgery procedure. That was something that did not appeal to this young woman, and she was thrilled to hear that a guided implant was a great treatment possibility. Some would consider a three-unit bridge, but I would only use this as a last resort. I also don't consider a Maryland bridge to be a viable long-term, fixed solution for this case.

The optimal treatment is to place an implant and leave the impacted canine undisturbed. Her implant experience was reflective of a flawlessly executed, guided implant placement that went exactly as planned. Her reaction to a 30-minute procedure under local anesthesia was, "That's it? I don't know why I was so nervous!" The chair time had been substantially reduced, and I even captured a smile photograph to finish off the visit.
The implant was planned and placed accordingly to be embedded by approximately 2 mm of buccal bone. This should ensure marginal bone stability for long-term success. A resonance frequency analysis with an Osstell device was used to confirm adequate bone-to-implant contact. The implant stability quotient (ISQ) value was 70, which meant that superior initial stability was achieved, verifying objectively that this implant could be loaded.
The patient and I discussed a provisional restoration with a noncontacting fixed tooth before commencing with surgery. A Cerec (Sirona) screw-retained Telio CAD hybrid abutment crown (Ivoclar Vivadent) was fabricated preoperatively and torqued into replace to restore her missing canine. This case illustrates how imaging influenced the clinical decision-making process and provided verification that an immediate implant was indeed possible.

'I was up all night'
 Emergency Schick 33 periapical radiograph.
Emergency Schick 33 periapical radiograph.The second case is of a 70-year-old patient of record who called early on a Monday morning and stated that he was up all night in severe pain. His chief complaint was pain in the lower right quadrant. On examination, I determined that his swelling spanned from the lower right lateral incisor to the second premolar, with concomitant pain to palpation and percussion. A Schick 33 (Sirona) periapical radiograph was taken, revealing the lower right canine as the culprit.
A previously treated endodontic tooth was failing. On initial review, I considered dismantling and retreating. The fill appeared to be short of the apex, but because of the extent of the swelling and level of pain, I wanted to evaluate in an enhanced 3D scan. The imaging led to my referral of this patient to an oral surgeon for an apicoectomy in an effort to retain this tooth.
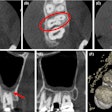
Interestingly, the tangential view was similar to the periapical view, but the cross-sectional view influenced my decision.
 Galileos scan that influenced referral.
Galileos scan that influenced referral.Looking carefully, one can see that the fill was well-done, and the buccal lingual tooth length was not the same in the horizontal plane. I did not feel that retreatment could improve this situation. An extraction and bone graft would not be the first choice, as his dentition was extremely crowded in this area. Crown and bridge also would be challenging to say the least.
 Apicoectomy completed at oral surgeon's office.
Apicoectomy completed at oral surgeon's office.The tooth was treated with an apicoectomy and retrograde filling, which resolved his symptoms within a few days. He thanked me on a follow-up appointment for not performing any unnecessary treatment that would not have solved his problem.
Having the technology available enables me to make clinical decisions at a higher level, directly benefiting my patients. Improving the doctor-patient relationship is a big reason for practice growth by creating patient advocates for better dentistry. Knowing what I can comfortably treat at the standard of care is most important when deciding whether to treat or refer.
I think these examples are illustrative of how I approach my decision-making selections, always keeping in mind to do no harm. I will continue to be a fervent advocate for the implementation and utilization of 3D imaging for all 21st century dental practices so that we dentists can provide evidence-based solutions and proposals to better our patients' health and lives. My journey continues. ...
Anthony Ramirez practices in Brooklyn, NY. He can be reached at [email protected] or via his website.
The comments and observations expressed herein do not necessarily reflect the opinions of DrBicuspid.com, nor should they be construed as an endorsement or admonishment of any particular idea, vendor, or organization.